JACC:冠状动脉左主干疾病的预测因素有哪些?
2022-02-19 MedSci原创 MedSci原创
在中度或重度缺血患者中,临床和压力测试参数对CTA上的LMD有中等预测作用。
冠状动脉疾病(coronary artery disease,CAD)是指冠状动脉血流减少所致的心脏病,最常见病因为动脉粥样硬化。临床表现包括无症状性心肌缺血, 心绞痛, 急性冠脉综合征 (不稳定性心绞痛, 心肌梗死),心源性猝死。
CAD诊断主要依据症状、心电图及负荷试验,有时需结合冠脉造影。预防主要通过改变可逆性危险因素(如血脂异常、高血压、体力活动缺乏、肥胖、糖尿病和吸烟)。治疗包括各类药物及非药物手段,以减少心肌缺血、恢复或改善冠脉血流。
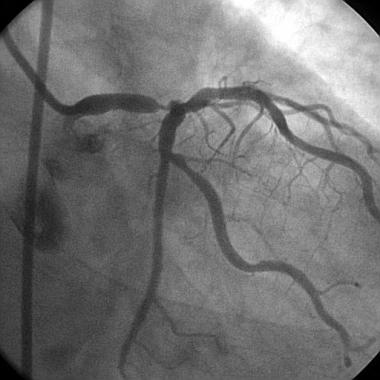
在所有接受冠状动脉造影的患者中,有4%-6%的患者存在严重的冠状动脉左主干病变(LMCAD),严重定义为冠状动脉造影显示狭窄超过50%。大约70%的LMCAD患者同时合并冠状动脉多支病变。

检测直径≥50%的狭窄左主冠状动脉疾病(LMD)具有预后和治疗的意义。无创压力成像或运动耐力测试(ETT)是检测阻塞性冠状动脉疾病的最常用方法,但LMD的压力测试标志物仍未确定。
为了利用临床和压力测试参数,确定在冠状动脉计算机断层扫描(CTA)上检测到的LMD的标志物,来自英国诺斯威克公园医院-皇家布朗普顿医院的专家开展了相关研究,结果发表在JACC杂志上。
这是对ISCHEMIA(医疗和侵入性方法的健康效果比较国际研究)的事后分析,包括随机和非随机参与者,他们在非成像ETT、应激核心肌灌注成像或应激超声心动图后的CTA排除了LMD的局部确定中度或重度缺血。之前有CABG术病史的患者被排除在外。
在5146名参与者中(平均年龄63岁,74%为男性),414人(8%)患有LMD。LMD的预测因素是年龄较大(P < 0.001),男性(P < 0.01),以前没有心肌梗死(P < 0.009),压力超声心动图上左心室的短暂缺血性扩张(P = 0.05),ETT上ST段压低的程度(P = 0.004),以及ETT上达到的代谢峰值当量(P = 0.001)。这些模型对LMD的预测作用一般(C-index 0.643和0.684)。
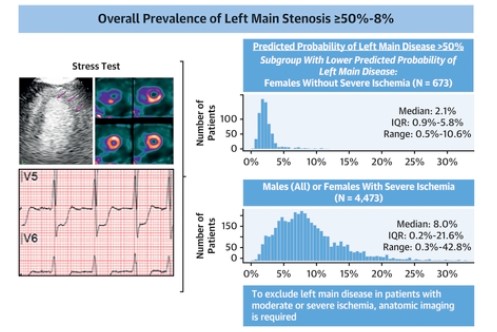
在中度或重度缺血患者中,临床和压力测试参数对CTA上的LMD有中等预测作用。对于大多数中度或重度缺血的患者,需要通过解剖学成像来排除LMD。
参考文献:
Predictors of Left Main Coronary Artery Disease in the ISCHEMIA Trial. J Am Coll Cardiol. 2022 Feb, 79 (7) 651–661
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#左主干#
73
#JACC#
58
#预测因素#
73
#ACC#
74
一篇好文章,确实受益匪浅
80