抑制 c-Myc 的 Hyper-O-GlcNAcylation 通过减轻角质形成细胞功能障碍加速糖尿病伤口愈合
2022-03-04 MedSci原创 MedSci原创
这些发现使 c-Myc 和 O-GlcNAc 成为糖尿病伤口的潜在治疗靶点。
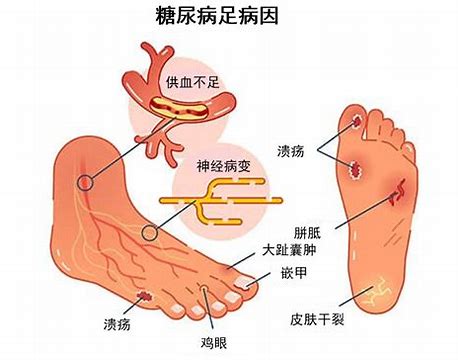
以延迟愈合为特征的糖尿病足溃疡是糖尿病的主要并发症之一。已发现表皮角质形成细胞功能障碍在糖尿病伤口愈合能力差中起关键作用。在本研究中,williamhill asia 旨在探讨 c-Myc 及其 O-连接的 N-乙酰氨基葡萄糖 (O-GlcNAc) 糖基化 (O-GlcNAcylation) 修饰与糖尿病伤口中角质形成细胞功能障碍之间的关系。
图1 文章来源
研究团队采集了临床创面标本,并建立糖尿病大鼠全层皮肤缺损创面模型。采用H&E染色观察创面再上皮化,免疫组化检测增殖细胞核抗原、转谷氨酰胺酶1、loricrin、c-Myc和O-GlcNAc的表达。
观察过表达或敲低c-Myc后人永生化表皮细胞(HaCaT)细胞增殖、迁移和分化的功能变化。使用免疫沉淀和邻近连接测定证实了 c-Myc 的 O-GlcNAcylation。使用放线菌酮测量c-Myc蛋白的稳定性。
在糖尿病伤口上局部应用抑制 c-Myc 或 O-GlcNAc 的化合物后,观察到伤口愈合。
结果显示,糖尿病伤口边缘的角质形成细胞具有增殖分裂活跃、迁移缓慢、分化差的特点。
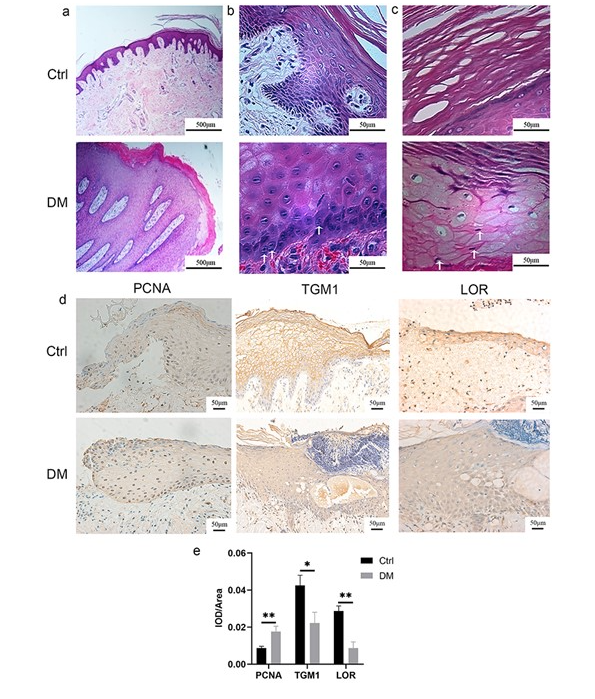
图2糖尿病患者伤口边缘的表皮角质形成细胞以增殖活跃、迁移缓慢和分化功能障碍为特征。
在糖尿病大鼠伤口边缘的 30 mM 葡萄糖和角质形成细胞中培养的 HaCaT 细胞中也观察到了类似的现象。
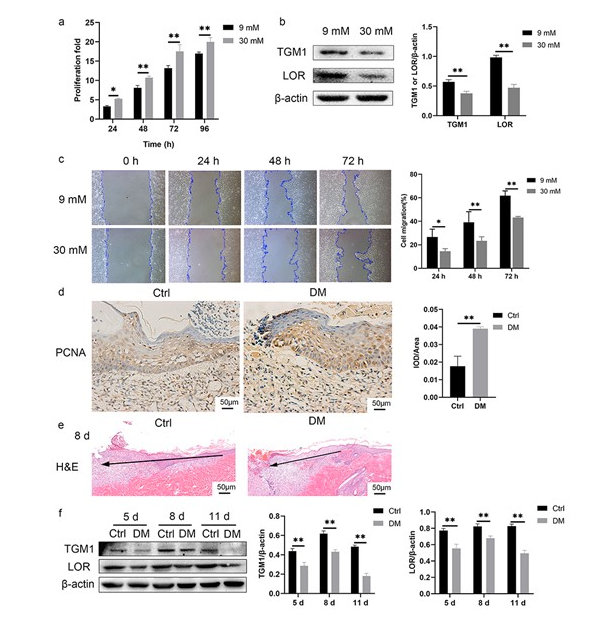
图3HaCaT 细胞在 30 mM 葡萄糖和大鼠糖尿病伤口边缘的角质形成细胞中培养,表现出活跃的增殖、缓慢的迁移和分化功能障碍。
c-Myc 在糖尿病大鼠、患者伤口边缘的角质形成细胞和用 30 mM 葡萄糖培养的 HaCaT 细胞中的表达增加。
c-Myc 表达增加促进增殖,同时抑制 HaCaT 细胞的迁移和分化,抑制 c-Myc 促进糖尿病伤口愈合。
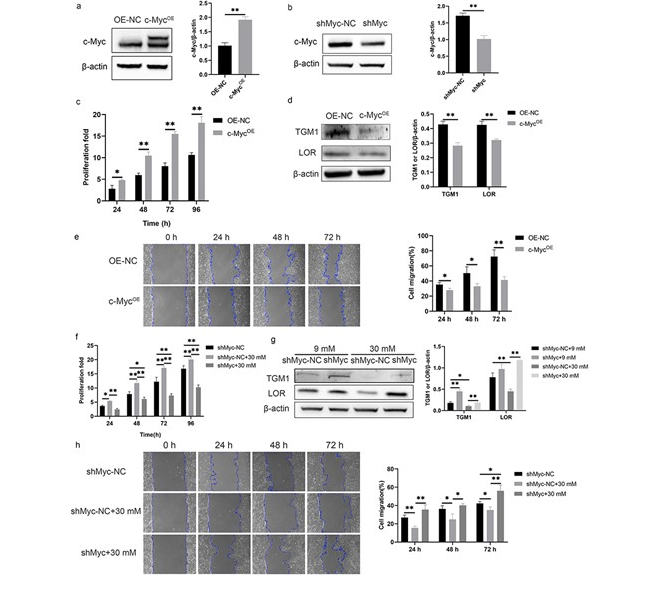
图4c-Myc 促进增殖并抑制 HaCaT 细胞的迁移和分化。
用 30 mM 葡萄糖增加 c-Myc 的 O-GlcNAcylation 稳定了 c-Myc 蛋白。
抑制 O-GlcNAc 可改善角质形成细胞功能障碍并促进糖尿病伤口愈合。

图5c-Myc 的抑制促进了糖尿病伤口的愈合。
总而言之,这项研究首先评估了c-Myc O-GlcNAcylation的调节可能影响糖尿病伤口的愈合。c-Myc 表达增加促进异常增殖并抑制糖尿病伤口边缘角质形成细胞的迁移或分化。在高葡萄糖糖尿病状态下增加的 c-Myc 的 O-GlcNAcylation 稳定了 c-Myc 蛋白。抑制 c-Myc 或 O-GlcNAc 可缓解糖尿病伤口愈合延迟。
这些发现使 c-Myc 和 O-GlcNAc 成为糖尿病伤口的潜在治疗靶点。
原始文章:
Jie Zhang, Peilang Yang, Dan Liu, Min Gao, Jizhuang Wang, Tianyi Yu, Xiong Zhang, Yan Liu, Inhibiting Hyper-O-GlcNAcylation of c-Myc accelerate diabetic wound healing by alleviating keratinocyte dysfunction,Burns & Trauma, Volume 9, 2021, tkab031
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言





.jpg)









#PE#
62
#MYC#
67
#伤口愈合#
85
#功能障碍#
61
#c-myc#
56
#细胞功能#
55