JACC:CTD患者6MW负荷超声心动图预测未来显性肺动脉高压
2015-07-21 崔倩 译 MedSci原创
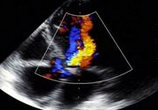
结缔组织病(CTD)患者早期检测肺动脉高压(PH)是至关重要的,这样可以确保患者的疾病及时得到治疗。运动负荷测试已经用于筛选患者以试图识别出早期的PH。最近的研究已经描述了异常平均肺动脉压(mPAP)-心输出量(Q)的反应作为具有评估疾病状态的可能性。 这项研究推测,通过6分钟步行(6MW)负荷超声心动图获得的肺循环压力 - 流的关系会更好地描述PH的差异进展以
结缔组织病(CTD)患者早期检测肺动脉高压(PH)是至关重要的,这样可以确保患者的疾病及时得到治疗。运动负荷测试已经用于筛选患者以试图识别出早期的PH。最近的研究已经描述了异常平均肺动脉压(mPAP)-心输出量(Q)的反应作为具有评估疾病状态的可能性。
这项研究推测,通过6分钟步行(6MW)负荷超声心动图获得的肺循环压力 - 流的关系会更好地描述PH的差异进展以及随访期间预测PH的发展。
研究人员对78例CTD患者在基线和随访期间进行了前瞻性地6MW应激超声心动图研究(年龄58±12岁;9%为男性)。所有患者每年进行超声心动图的随访研究,长达5年时间。
在32个月(范围:15〜62个月)的中位随访期间内,16例患者达到了PH发展的临床终点,随访期间无死亡病例。所有16例患者的PH通过右心脏导管(mPAP≥25mmHg,肺毛细血管楔压≤15mmHg)证实存在。在Cox比例风险生存模型中,6MW的距离(危险比[HR]:0.99;P=0.010),早期舒张三尖瓣环运动速度(HR:0.79;P=0.025),以及通过6MW应激得到的ΔmPAP/ΔQ(HR :1.10;P=0.005)均与PH的发展有关。在连续Cox模型中,在6MW距离(卡方,6.6)的基础上,通过ΔmPAP/ΔQ模型得到改善(卡方:14.4;P=0.019)。使用受试者工作特征曲线,研究人员发现,预测肺动脉高压发展的ΔmPAP/ΔQ的最佳截止值是>3.3mmHg/L/min。
该6MW负荷超声心动图无创性的提供了CTD患者PH发展的增量预后价值。这是一个单中心前瞻性队列研究。还需较大的多中心研究来证实这一结果。
原始出处:
Kenya Kusunose,Hirotsugu Yamada,Junko Hotchi,et al.Prediction of Future Overt Pulmonary Hypertension by 6-Min Walk Stress Echocardiography in Patients With Connective Tissue Disease,JACC,2015.7.21
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#心动图#
52
#动脉高压#
57
#JACC#
64
#ACC#
50