Brit J Anaesth :非心脏手术患者术中低血压与持续性急性肾病相关
2022-05-18 MedSci原创 MedSci原创
术中低血压与持续性而非迟发性急性肾脏疾病相关。这两种急性肾病似乎都与增加的医疗保健利用水平相关。纠正术中低血压是减少术后肾损伤和降低相关费用的潜在措施。
围手术期急性肾损伤在手术患者中很常见。它在接受重大非心脏手术的患者中很常见,发生率为6.3-13.4%,也是患者发病和死亡的主要原因。虽然术中低血压与术后急性肾损伤有关,但术中低血压与急性肾脏疾病之间的联系尚未明确。
近日,麻醉疼痛领域权威杂志British Journal of Anaesthesia上发表了一篇研究文章,研究人员利用从美国电子健康记录数据库中提取的非心脏、非产科手术数据进行了一项回顾性多中心队列研究。

该研究的主要观察性结局是根据三个平均动脉压(MAP)阈值(≤75、≤65和≤55mmhg)来定义的术中低血压与以下两个急性肾脏疾病亚型之间的相关性:(i)持续性(术后7天内发生的急性肾损伤,术后8至90天持续存在)和(ii)迟发性(7天内未发生急性肾损伤的肾损害,术后8至90天发生急性肾损伤)。该研究的次要结局包括急性肾脏疾病亚型或无急性肾脏疾病患者的医疗资源利用情况。
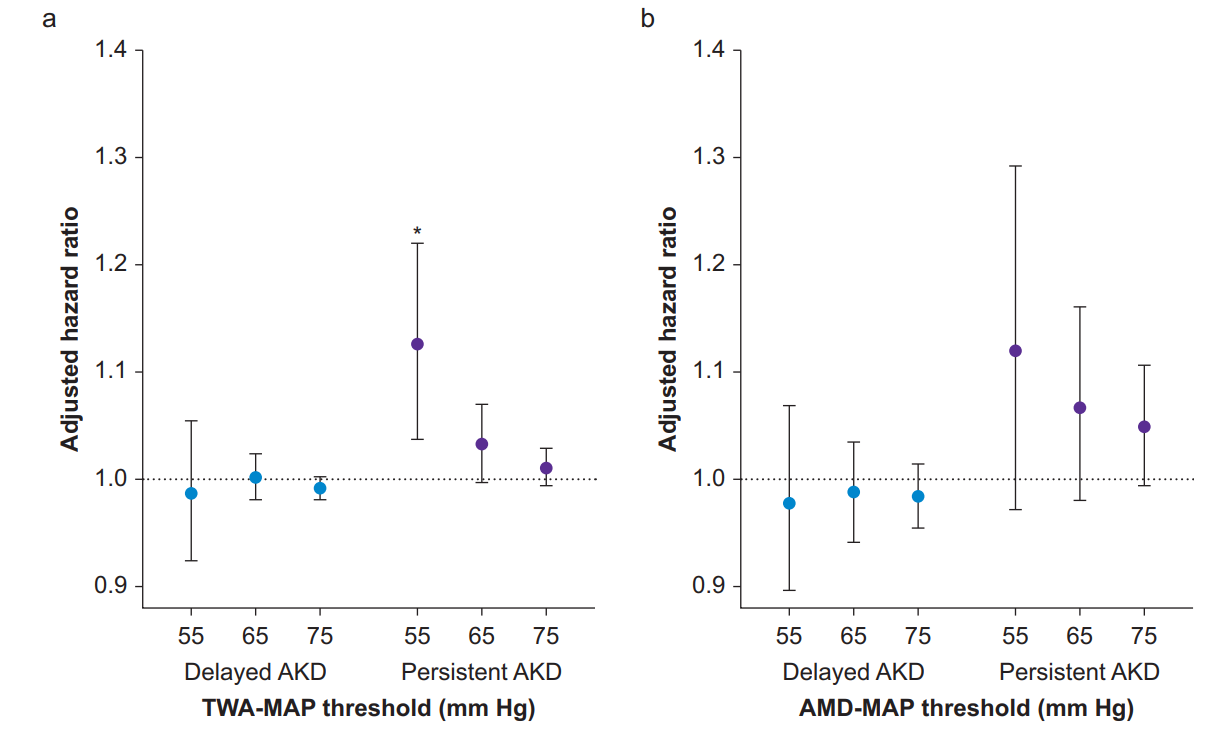
该研究共有112912名手术患者符合纳入标准。研究人员观察到迟发性急性肾脏疾病为2.2%,持续性急性肾脏疾病为0.6%。术中低血压与持续急性肾脏疾病显著相关,MAP≤55mmhg(风险比为1.1;95%置信区间:1.38~1.22;P<0.004)。然而,对于任何MAP阈值的术中低血压与延迟急性肾脏疾病均无显著相关性。与没有急性肾脏疾病的患者相比,延迟或持续性急性肾脏疾病患者在医院和重症监护住院期间的医疗资源利用率更高。
由此可见,术中低血压与持续性而非迟发性急性肾脏疾病相关。这两种急性肾病似乎都与增加的医疗保健利用水平相关。纠正术中低血压是减少术后肾损伤和降低相关费用的潜在措施。
原始出处:
Andrew D. Shaw.et al.Intraoperative hypotension is associated with persistent acute kidney disease after noncardiac surgery: a multicentre cohort study.British Journal of Anaesthesia.2022.https://www.bjanaesthesia.org/article/S0007-0912(22)00157-X/fulltext
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#EST#
72
#持续性#
63
#非心脏#
56
#ANA#
54
学习了
65
#低血压#
74
#非心脏手术#
71
#术中低血压#
71
学习了,谢谢分享
61