EMBO Mol Med :AAV病毒基因疗法,成功挽救先天性耳聋
2020-12-31 生物世界 Bio生物世界
耳聋,是全世界最常见的感官障碍。根据世界卫生组织(WHO)统计,当今全世界约有十亿人存在听力损失,并且预计这个数字在未来几十年中翻番。
耳聋,是全世界最常见的感官障碍。根据世界卫生组织(WHO)统计,当今全世界约有十亿人存在听力损失,并且预计这个数字在未来几十年中翻番。
其中,每200名儿童中就有1名患有先天性听力障碍,每1000名儿童中就有1名耳聋。这些听力障碍和耳聋,大约一半是由基因突变引起的。目前已经发现约120种与遗传性耳聋相关的基因。
几年前,特拉维夫大学 Karen Avraham 教授团队在两个以色列家庭中发现了一种罕见耳聋,这种遗传性耳聋是由于 SYNE4 基因突变引起,这种罕见耳聋此后在土耳其和英国也有发现。
从父母哪里遗传了 SYNE4 基因突变的孩子在出生时听力正常,但在儿童时期开始逐渐丧失听力,该基因突变会导致内耳耳蜗内毛细胞中细胞核定位错误,导致毛细胞变性死亡,最终导致听力完全丧失。
近日,以色列特拉维夫大学的研究人员在 EMBO Molecular Medicine 杂志发表了题为:Neonatal AAV gene therapy rescues hearing in a mouse model of SYNE4 deafness 的研究论文。
研究团队使用腺相关病毒(AAV)载体作为基因治疗载体,成功将正确版本的SYNE4 基因递送到 SYNE4 基因敲除的耳聋小鼠模型,能够有效防止小鼠的听力下降,研究结果表明AAV基因治疗是治疗遗传性耳聋的有力手段,在治疗儿童遗传性耳聋领域有着巨大应用前景。
研究团队使用腺相关病毒(AAV)载体作为基因治疗载体,具体血清型为AAV9-PHP.B。AAV9-PHP.B是通过定向体内进化工程开发并合成的AAV血清型,对内耳毛细胞和外耳毛细胞均有很高的转导效率。
将正确版本的 SYNE4 基因通过注射递送到SYNE4 基因敲除(KO)的小鼠模型的内耳,腺相关病毒载体将 SYNE4 基因递送到内耳毛细胞,并在毛细胞中表达。
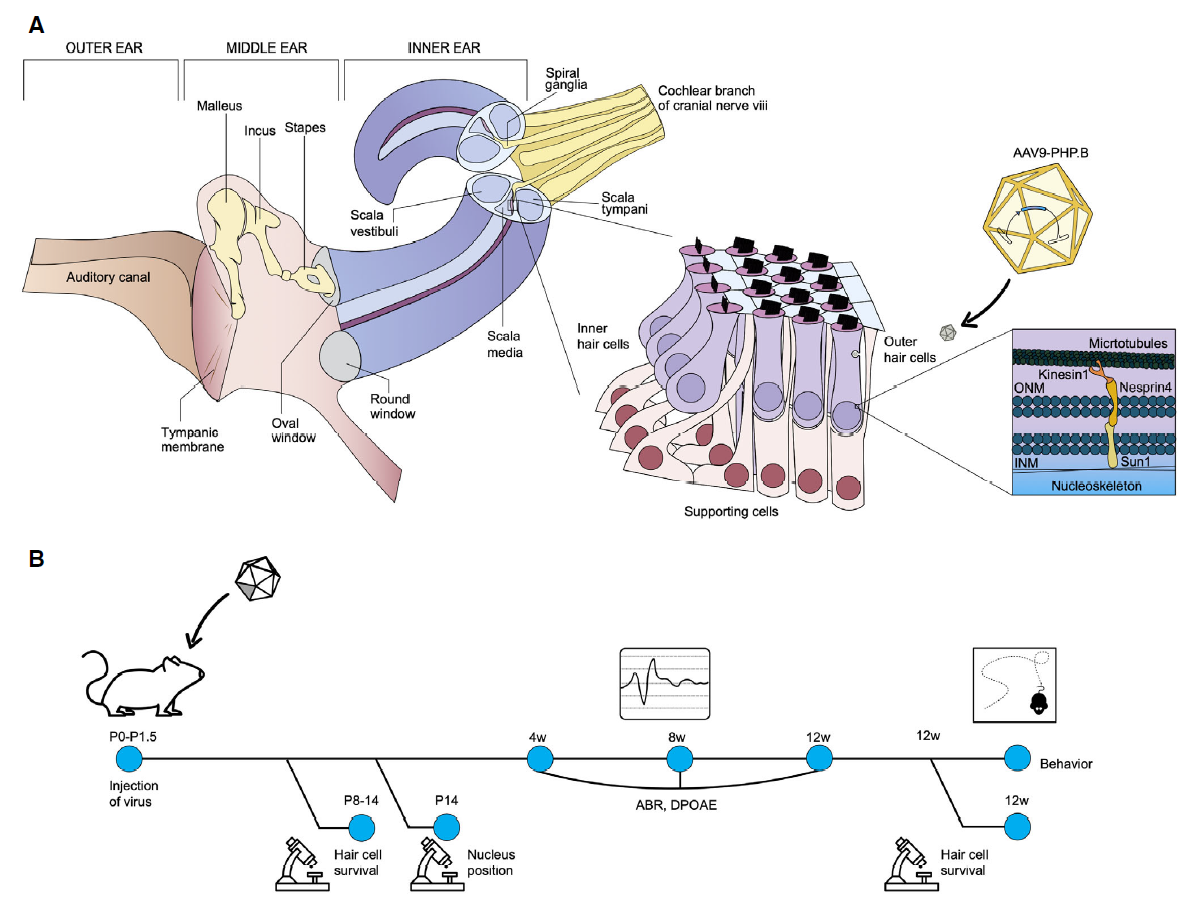
研究团队在模型小鼠出生后不久进行了这种基因治疗,使用生理和行为测试来监测小鼠的听力。研究结果表明,经过治疗的耳聋小鼠的听力恢复正常,其敏感性几乎与没有该基因突变的健康小鼠相同。

总的来说,研究团队开发的这种AAV基因疗法,对耳聋小鼠的听力恢复程度令人印象深刻。这项研究清楚地表明,基因治疗可以成功地应用于遗传性听力损失的小鼠模型,表明基因疗法在治疗遗传性耳聋方面有巨大潜力。
原始出处:
Shahar Taiber , Roie Cohen , Ofer Yizhar-Barnea,et al.Neonatal AAV gene therapy rescues hearing in a mouse model of SYNE4 deafness. EMBO Mol Med . 2020 Dec 22;e13259. doi: 10.15252/emmm.202013259.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#先天性耳聋#
60
#AAV#
87
#先天性#
58
#Med#
54