JACC:替格瑞洛联合阿司匹林对PCI术后的抗血栓影响
2020-02-22 不详 MedSci原创
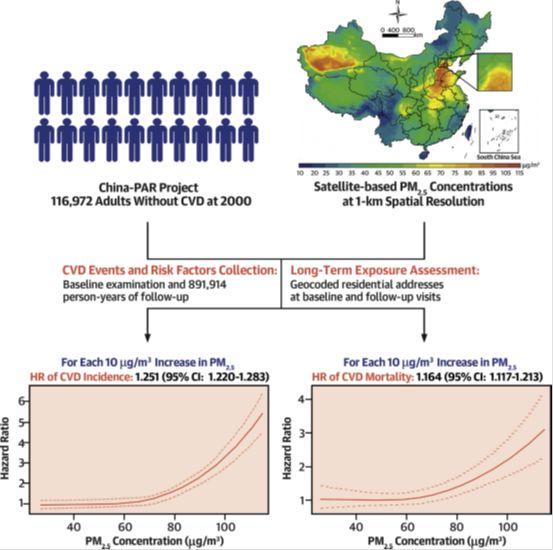
本研究的目的旨在比较和评估替格瑞洛以及替格瑞洛联合乙酰水杨酸(ASA)对接受药物洗脱支架冠脉介入治疗患者的抗血栓形成效果。TWILIGHT临床试验将接受PCI治疗患者在3个月的双重抗血栓形成治疗中随机分成替格瑞洛+安慰剂治疗和替格瑞洛联合ASA治疗,主要终点事件是花生四烯酸刺激后的血栓大小。最终共纳入分析了51名患者,随访结束后的血栓面积在两组患者中无明显差异(p=0.22),在对环氧化酶-1阻断
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#JACC#
62
#PCI术#
59
#ACC#
52
#PCI术后#
0
#抗血栓#
70