Cardiovasc Diabetol:2型糖尿病患者累积甘油三酯-葡萄糖指数与主要心血管不良事件的相关性
2022-09-15 从医路漫漫 MedSci原创
甘油三酯-血糖(TYG)指数是从空腹血糖(FBG)和甘油三酯(TG)水平得出的一个参数
背景:心血管疾病(CVD),包括冠心病、脑血管疾病和外周动脉疾病,是糖尿病患者发病率和死亡率的主要原因。最近对2型糖尿病(T2 DM)患者进行的心血管结果事件试验表明,包括心肌梗死(MI)、中风和心血管死亡在内的主要不良心血管事件(MACE)的发生率从9.4%到12.1%不等,每年与糖尿病相关的心血管支出估计为373亿美元。因此,评估和控制个体心血管危险因素以预防或减缓糖尿病患者的心血管疾病是重要的。胰岛素抵抗(IR)是T2 DM的病理生理学基础,通常与高血压、血脂异常和血糖异常有关。此外,炎症和血栓标志物与IR相关,从而导致炎性动脉粥样硬化血栓综合征。因此,长期IR不仅会引起高血糖和高血压,还会导致血脂代谢和抗凝机制的异常,从而增加血栓形成的风险。此外,一些研究表明,糖尿病患者的冠状动脉粥样硬化病变与更多的动脉粥样硬化、巨噬细胞浸润和斑块内血栓相关;这表明糖尿病患者的IR是炎性动脉粥样硬化血栓形成过程的生物标志物,将MACEs与T2 DM的潜在机制联系起来。因此,长期监测和控制胰岛素抵抗可能有助于预防2型糖尿病患者的急性心肌梗死。
在临床环境或大型人群研究中,由于当前金标准方法(胰岛素抵抗的正常血糖钳和稳态模型评估[HOMA-IR])中的一些限制,IR测量可能具有挑战性。甘油三酯-血糖(TYG)指数是从空腹血糖(FBG)和甘油三酯(TG)水平得出的一个参数,于2008年首次提出,被认为是一个令人信服的IR指标。TYG指数已被证明与正常血糖-高胰岛素钳夹形成相关,因此具有与HOMA-IR相似的有效性。此外,TYG指数的优势是在任何临床环境下都很容易获得,从而使williamhill asia 的发现得到广泛应用。因此,在这项特殊分析中,TYG指数被用作IR的生物标记物,以研究其与T2 DM患者发生急性心肌梗死风险的关系。最近,相当多的研究提供了强有力的统计证据,表明TYG指数可能有助于识别患T2 DM的风险,并与心血管疾病的发展和预后相关。一项队列研究(6078名年龄>60岁的参与者)表明,TYG指数最高的四分位数的参与者发生心血管事件的风险高出72%。使用来自国家健康信息数据库的数据,平均随访时间为8.2年,Hong等人进一步证实,TYG指数四分位数最高的参与者中风和心肌梗死的风险更高,独立于其他传统的心血管风险因素。此后,TYG指数与不同类型的CVD之间的关系被连续揭示。然而,大多数关于高TYG指数和心血管结局之间关系的观察性研究都集中在单个时间点测量的TYG指数值上,很少有研究表征长期TYG指数及其对T2 DM患者MACEs的影响。
更重要的是,控制不佳的血脂和血糖水平会影响心血管事件的缓慢进展。长期与当代相比,血脂和血糖水平可能更显著地影响心血管事件的发生。此外,心血管危险因素的累积暴露已被证明可以预测不利的长期心血管结果和死亡率的风险,独立于基线风险因素水平。先前的研究表明,TYG指数较高的暴露时间越长,心血管疾病风险增加的可能性越大。尽管williamhill asia 之前的研究也表明TYG指数的高长期轨迹与MACES的发生显著相关,但尚不清楚累积TYG指数是否是T2 DM患者未来MACES的更强风险因素。在目前的研究中,williamhill asia 假设在随访期间长期暴露于高TYG指数可能会影响T2 DM患者MACES的发展。
目的:使用控制糖尿病心血管风险的行动(ACCORD)和ACCORD后续研究的数据,williamhill asia 评估了早期随访期间累积TYG指数暴露与以后生活中MACES发生率之间的关系。
方法:对控制糖尿病心血管风险行动(ACCORD)试验的事后分析评估了来自研究数据库的患者(T2DM > 3个月)的累积TyG指数和MACE数据。在基线和前四次就诊时,对5695名没有经历过MACEs的参与者进行了五次空腹血糖和甘油三酯测量。对TyG指数的累积暴露计算为每个时间间隔的平均TyG指数值的加权和(值×时间)。多变量校正Cox比例风险模型和限制性三次样条分析用于确定累积TyG指数和MACEs之间的关系。进一步评估累积TyG指数的增量预测值。
结果:在平均5.09年的随访中,发生了673例(11.82%)mace,包括256例(4.50%)心血管疾病(CVD)死亡,288例(5.06%)非致命性心肌梗死(MIs)和197例(3.46%)中风。随着累积TyG指数四分位数的增加,发生MACEs的风险增加。在调整了多个潜在混杂因素后,累积TyG指数非常高的组相对于累积TyG指数低的组,总体MACEs、CVD死亡和非致命性MI的风险比分别为1.59 (95%可信区间[CI],1.17-2.16)、1.97(95% CI 1.19-3.26)和1.66(95% CI 1.02-2.70)。限制性三次样条分析也显示,随着累积TyG指数的增加,MACEs的风险也逐渐增加。在MACEs的传统风险模型中增加累积TyG指数改善了C-统计、净再分类改善值和综合鉴别改善值。
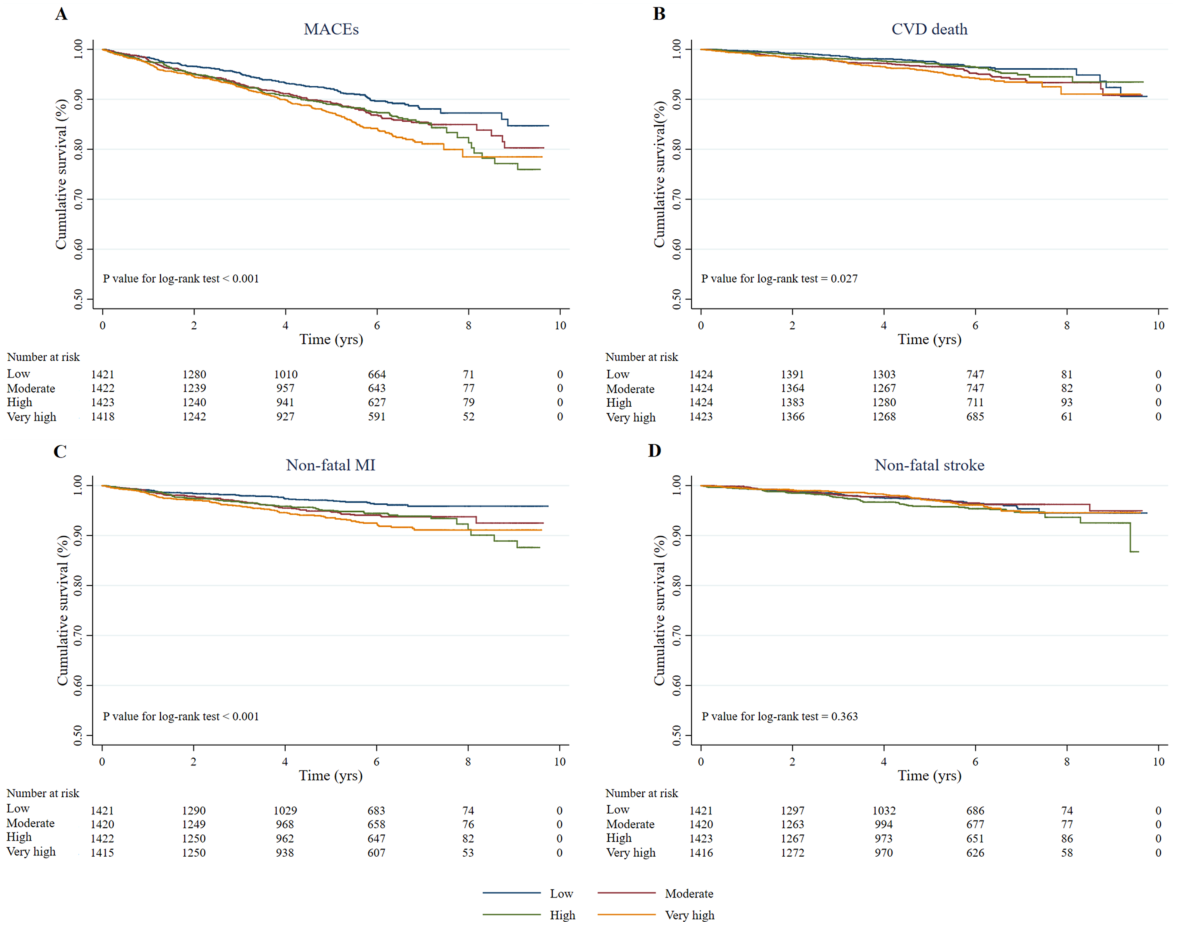
图1基于累积TYG指数四分位数的MACES和个体预后的Kaplan-Meier生存曲线。A、b、心血管疾病相关死亡;c、非致命性心肌梗死;d、非致命性中风。MACES主要心血管不良事件,甘油三酯-葡萄糖
表1累积TYG指数的事件风险和个人结果
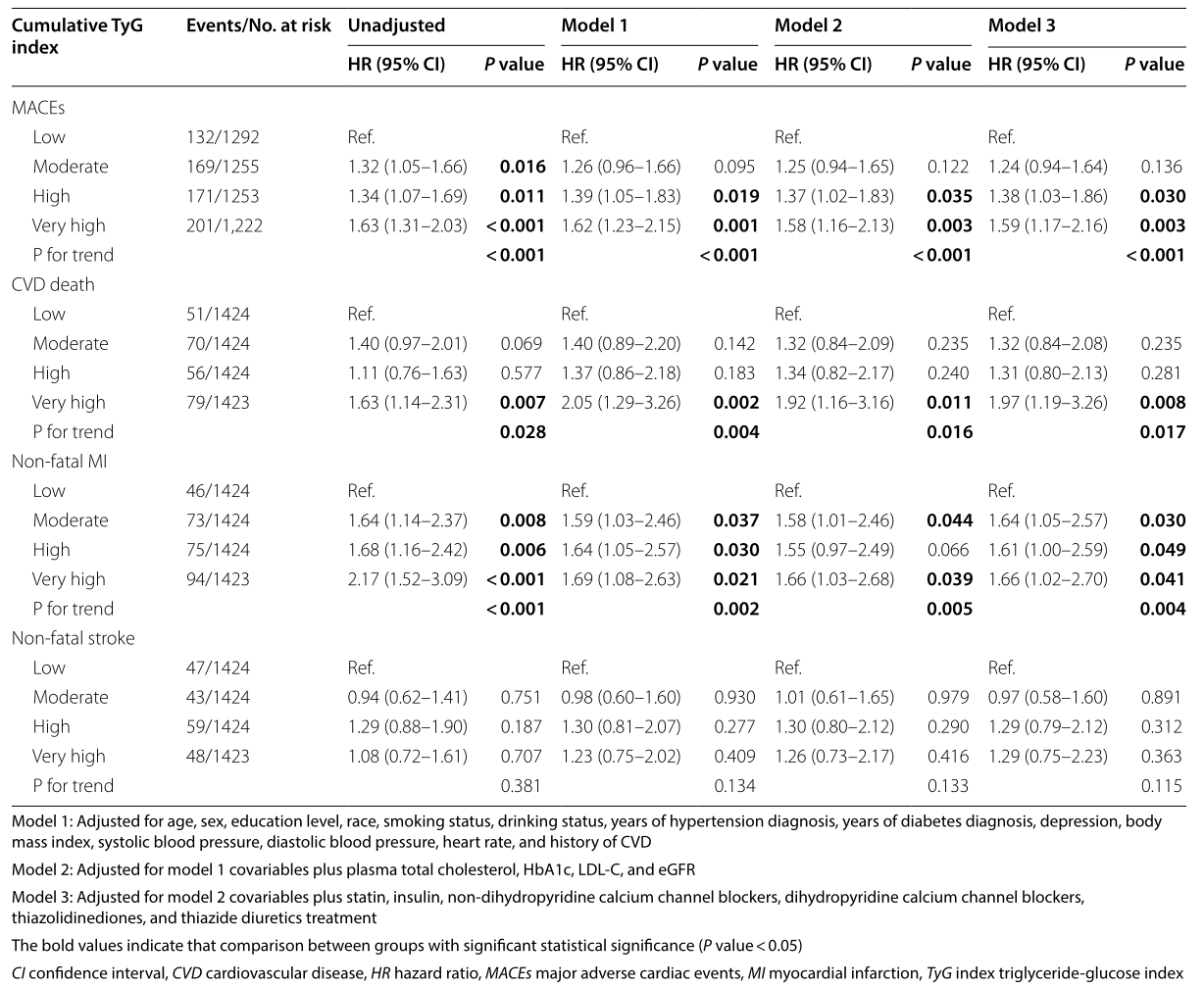
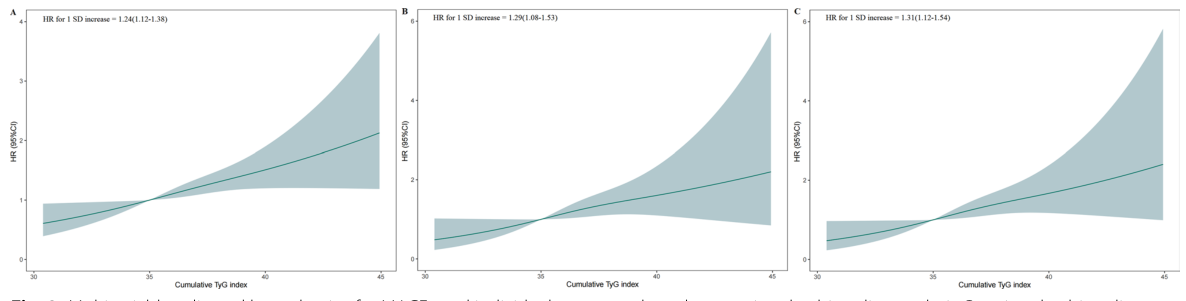
图2基于限制性三次样条法的MACES和个体结果的多变量调整风险比。限制三次样条分析在甘油三酯-葡萄糖(TYG)指数变化的第25、50、75和95个百分位数处有5个结点。A急性心肌梗死;b心血管疾病相关死亡;c非致命性心肌梗死。CI可信区间、心血管疾病、心率危险比、MACES主要不良心血管事件、SD标准差、甘油三酯-血糖
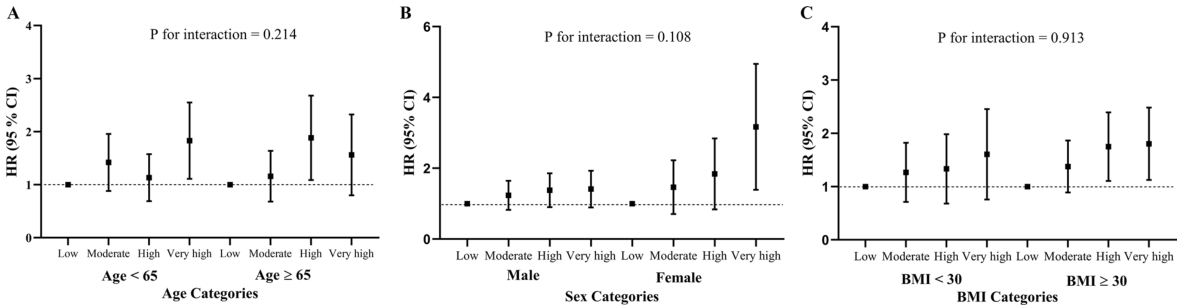
图3累积甘油三酯-血糖(TYG)指数与MACES关系的亚组分析。研究人群按年龄(<65岁与≥65岁)、性别(男性与女性)和体重指数(BMI;<30 kg/m2与≥30 kg/m2)进行分层。在基线水平上对年龄、性别、教育水平、种族、吸烟状况、饮酒状况、高血压诊断年限、糖尿病诊断年限、抑郁、体重指数、收缩压、舒张压、心率、心血管病史、血浆总胆固醇、糖化血红蛋白、低密度脂蛋白胆固醇、表皮生长因子受体、他汀类药物、胰岛素、非二氢吡啶类钙通道阻滞剂、二氢吡啶类钙通道阻滞剂、噻唑烷二酮类药物和噻嗪类利尿剂治疗进行了调整。BMI体重指数、CI可信区间、心血管疾病、EGFR估计肾小球滤过率、HbA1c糖化血红蛋白、HR危险比、低密度脂蛋白胆固醇、MACES主要心血管不良事件、SD标准差、TYG甘油三酯-葡萄糖
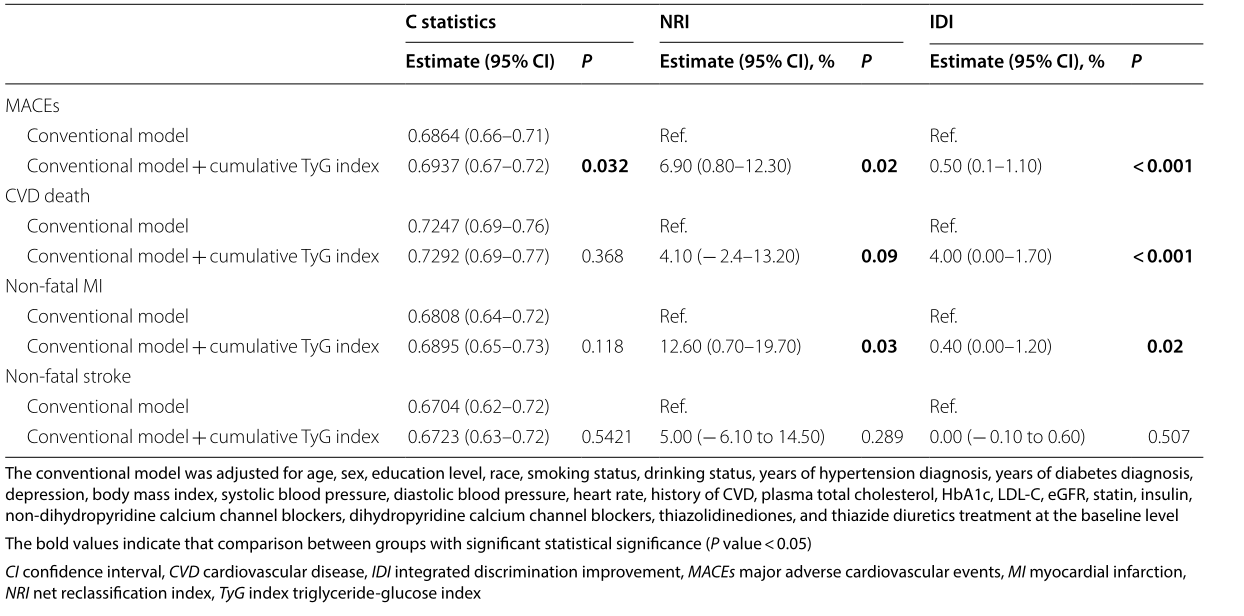
表2累计TYG指数增量预测值
结论:在T2 DM患者中,累积TYG指数独立地预测MACES的发生率,监测长期TYG指数可能有助于对MACEs进行风险分层和预后预测。
原文出处: Tai S, Fu L, Zhang N, et al.Association of the cumulative triglyceride-glucose index with major adverse cardiovascular events in patients with type 2 diabetes.Cardiovasc Diabetol 2022 08 23;21(1)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#DIA#
64
#BET#
61
#ASC#
52
#相关性#
48
#2型糖尿病患者#
56
#糖尿病患者#
92
#心血管不良事件#
58