肝硬化门静脉高压症围术期处理策略
2016-09-20 佚名 中华消化外科杂志
作者 上海交通大学医学院附属仁济医院 吴志勇 陈炜 肝硬化门静脉高压症合并食管胃底静脉曲张破裂出血的围术期处理是否合理,直接影响疾病治疗效果和患者生命质量,临床医师应高度重视。根据患者个体特点,选择合理的治疗方法,是提高门静脉高压症治疗效果的关键,也是精准医疗的核心。1 术前准备 肝硬化门静脉高压症术前除常规评估全身重要脏器,如心、肺、肾和心脑血管等功能外
作者 上海交通大学医学院附属仁济医院 吴志勇 陈炜
肝硬化门静脉高压症合并食管胃底静脉曲张破裂出血的围术期处理是否合理,直接影响疾病治疗效果和患者生命质量,临床医师应高度重视。根据患者个体特点,选择合理的治疗方法,是提高门静脉高压症治疗效果的关键,也是精准医疗的核心。
1 术前准备
肝硬化门静脉高压症术前除常规评估全身重要脏器,如心、肺、肾和心脑血管等功能外,还需特别评估肝硬化病因、肝脏储备功能、门静脉高压症程度、肝脏和门静脉系统血流动力学状况。
1.1 肝硬化病因学评估
应常规行甲、乙、丙、戊型等各类肝炎病毒血清学检查。若是由乙型病毒性肝炎后肝硬化引起,还应行HBV DNA值测定。若肝炎病毒血清学检查结果为阴性,还需行免疫学检查。若抗核抗体、抗平滑肌抗体、抗肝肾微粒体、抗可溶性肝抗原/肝胰抗原等指标检测结果为阳性,应怀疑自身免疫性肝病。抗线粒体抗体阳性则需考虑胆汁淤积性肝病。上述检查有助于肝硬化病因诊断。
1.2 肝脏储备功能评估
肝脏储备功能主要反映患者对手术的耐受性,目前普遍采用肝功能Child分级。肝功能Child A级患者,对手术耐受性好;Child B级患者,手术风险较大;Child C级患者,原则上不能行传统手术,只能拟行肝移植。若将该分级系统结合肝脏体积测定,更能准确反映肝脏储备功能。目前国内外测定肝脏体积常依靠肝脏CT检查。肝脏体积缩小不明显,即使肝功能较差,对手术耐受性仍较好。相反,若肝脏体积明显缩小,即使肝功能较好,但肝功能已处于临界状态,手术风险大。若将肝功能Child分级、肝脏体积测定和吲哚氰绿排泄试验综合应用,则能更准确评估肝硬化门静脉高压症患者肝脏储备功能,判断其手术耐受性。
肝硬化门静脉高压症患者肝脏明显萎缩、肝功能ChildC级时,常不能耐受常规手术,需考虑行肝移植治疗。
1.3 门静脉高压症程度评估
门静脉高压症程度评估包括确定脾功能亢进程度和静脉曲张程度。脾功能亢进程度评估依赖血液学检查,血常规WBC<2.0×109/L、PLT<30×109/L为重度脾功能亢进。该结果需多次测定,结果一致时才能确定。肝硬化患者重度脾功能亢进,且食管胃底静脉曲张较重,或仅有重度脾功能亢进,但伴有相应临床症状时,可考虑行脾切除+预防性断流术。
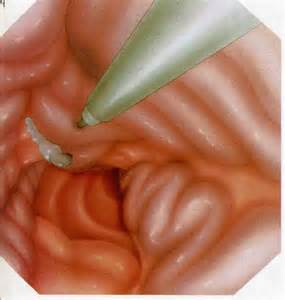
食管下段胃底静脉曲张程度评估需依靠内镜检查。内镜检查是诊断食管下段胃底静脉曲张的金标准。在急性出血期,通过内镜下曲张静脉套扎术或硬化剂注射控制出血,可减少出血对肝脏的损害。食管胃底曲张静脉直径>5mm,考虑大曲张静脉。
1.4 肝脏和门静脉系统血流动力学状况评估
术前肝脏和门静脉系统血流动力学状况评估主要依靠影像学检查。多普勒超声检查显示的门静脉入肝血流量结果迥异,其准确性受到质疑。但该方法可较准确测定门静脉血流方向。
CT血管成像或磁共振门静脉系统血管成像检查可了解门静脉系统解剖影像及血流动力学改变,显示血管解剖结构,反映流速、流量等功能状态,对了解门静脉系统干支直径、通畅性(血栓部位和程度等),侧支部位、直径、数目,以及肝脏血流灌注状态十分有用;也能很好地显示各血管间以及血管和相邻器官间的复杂空间关系和解剖形态,有效帮助临床医师选择正确的手术方式。因腹腔积液影响磁共振门静脉系统血管成像检查效果,故临床上CT血管成像检查应用更广泛。经肝动脉门静脉造影检查为有创性,目前几乎均可被上述无创检查替代。当侧支血管十分粗大,怀疑门静脉已成为流出道患者,可行肝动脉造影检查。若门静脉显影,则证明门静脉已成为流出道,许多手术方式受到限制,只能行门腔静脉、肠腔静脉侧侧分流术或架桥分流术,以及传统的脾肾静脉分流术等。
2 术中决策
术中探查,修正术前对肝脏储备功能及门静脉高压症程度的评估。若肝脏体积虽较大,但质地坚硬,不能耐受较大手术。腹膜后粗大侧支血管连成片状者,手术除需保护这些自发性侧支血管外,操作需十分小心,如不慎损伤,出血将较难控制。分流术不易成功者,通常只能行断流术,若脾周也有较多侧支血管,可能只结扎脾动脉。
虽然依据术前的血流动力学资料,可对门静脉高压症手术方式做出较为准确的选择,但需结合术中探查所见和门静脉压力再测定,重新评估和决策。
依据术中压力变化选择手术方式,首先必须保证FPP测定结果准确。传统的经胃网膜右静脉穿刺插管,导管不易进入肠系膜上静脉-门静脉,且每次取零点和采用水柱法读取数据不可靠,结果误差较大。此外,将导管连接压力换能器,零点固定在下腔静脉水平,可动态观察压力变化。除零点可能稍有误差外,不同手术阶段变化结果不受影响。FPP测定时段在开腹后、脾动脉结扎后、脾切除后、分流后和断流后。
2.1 断流术
断流术的合理性在于其直接针对引起出血的曲张静脉,手术较简单,同时维持了门静脉向肝血流。但断流术也存在一定弊端,如术后门静脉系统压力仍高,不可避免地形成脾-门静脉血栓,术后远期形成新的曲张血管,再出血率较高,为10%~20%。门静脉压力高,将进一步加重门静脉高压性胃病。术后诸如腹腔积液、腹腔感染、长时间发热、胃肠功能紊乱等并发症多。
目前,断流术种类较多。裘法祖教授倡导的贲门周围血管离断术安全、合理、有效、便捷,在我国已成为断流术的主流手术方式。近年来,杨镇教授提出了选择性断流术,手术操作同裘法祖教授倡导的方法,但保留胃左静脉主干和食管旁静脉,并保持门奇静脉自发形成分流的完整性,以期降低门静脉压力。由于保脾断流术不能降低门静脉压力和纠正脾功能亢进,其在肝硬化门静脉高压症治疗中的地位有待进一步考证。
2.2 分流术
分流术的优点在于从根本上分流了部分门静脉血流,降低了门静脉压力,继而减轻了食管胃底曲张静脉的血流负荷,防止破裂出血。其缺点在于有效的门体分流,导致肝血流量减少,可能引起肝功能进一步恶化,肝性脑病发生率增加。基于肝硬化门静脉高压症发病基础是肝内阻力增加和内脏血流量增多,且多数患者前者作用较大,因此,理论上分流术较合理。临床实践中门体分流术适应证为:(1)食管胃底曲张静脉粗大,且数目多。(2)肝硬化食管胃底静脉曲张内镜套扎术后复发出血。(3)门静脉高压性胃病出血。(4)术中发现胃壁明显增厚、水肿。(5)脾动脉结扎后FPP>20mmHg或行脾切除断流术后FPP≥22mmHg。
2.3 联合手术
在门静脉高压症手术中,若结扎脾动脉后FPP未能下降至<22mmHg,就应准备加行分流术,因为其后的手术操作不仅不会降低门静脉压力,反而会使其小幅度上升。脾切除+脾肾静脉分流+贲门周围血管离断术最为合理,其可纠正脾功能亢进,使静脉曲张减轻或消失。近年来笔者单位简化断流术操作,即完成脾肾静脉吻合后,将胃冠状动静脉缝扎,如存在高位异位侧支予以缝扎,而不是将食管下段及上半胃所有侧支离断结扎。这可减少手术创伤、术后出血量等并发症,并节约手术时间。此外,该手术后肝性脑病发生率约为12%,近年基本无发生,可能与抗病毒治疗有关。
3 术后处理
术后应严密监测患者生命体征,保持引流管通畅,注意观察引流量和颜色,无血性液体引出时,于术后3~4d拔除引流管。拔管前应检测引流液淀粉酶含量,以排除是否存在术中胰尾部误伤。此外,还应重视以下处理:(1)肝硬化患者肝脏储备功能下降,术后需积极行保肝治疗。(2)注意防治腹腔积液。(3)门静脉高压症术后发热多见,主要由各类积液引起,如胸腔积液、腹腔积液感染、膈下积液感染等。其他如导管、血液、呼吸道或尿路感染,需积极行病原学检查,选择合理抗菌药物治疗,并行相应引流处理。若排除了感染因素,则可能与门静脉系统血栓形成有关,非甾体类抗炎药物治疗有效。(4)肝硬化门静脉高压症不论采用何种手术方式,术后门静脉系统血栓形成率均相当高。(5)行脾切除术后,多数患者PLT迅速升高,在2周左右达到峰值,之后逐渐降低。因此,术后应严密监测患者凝血状态和PLT计数,尤其是后者。若PLT>800×109/L,应行抗凝、祛聚治疗,包括口服潘生丁和阿司匹林,静脉滴注低分子右旋糖酐、丹参,皮下注射低分子肝素等,可防止血栓进一步扩展。
4 结语
我国病毒性肝炎发病率极高,肝硬化患者众多,虽部分患者经肝移植得以治愈,但毕竟是少数,多数肝功能尚好或不愿行肝移植的患者仍需行各种非手术和传统手术治疗。非手术治疗无效时,在相当长一段时间内,传统手术仍居主导地位。不同患者肝硬化的病情发展阶段不同,治疗方案也应不同,应强调个体化治疗。因没有一种手术方式可适合所有患者,若手术方式选择不合理,可能对患者造成灾难性的后果。因此,笔者强调:依据门静脉血流动力学状况选择合理手术方式,才能使患者最大获益;完善的术前准备,根据血流动力学变化选择合适手术方式,积极的术后处理,才能获得最佳治疗效果。
摘自:《中华消化外科杂志》 第15卷第7期
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#围术期处理#
74
#门静脉高压症#
79
#静脉#
78
#处理策略#
68
#围术期#
55
#门静脉#
59