骨髓瘤治疗新进展,全新作用机制药物Selinexor(ATG-010)三种治疗方案入选更新版NCCN®多发性骨髓瘤诊疗威廉亚洲博彩公司
2020-12-16 医药魔方 医药魔方
12月15日,德琪医药有限公司(简称“德琪医药”)宣布,美国国家综合癌症网络(NCCN®)在最新版多发性骨髓瘤临床实践威廉亚洲博彩公司 (NCCN Guidelines®)中添加了三种selinexor(ATG-0
12月15日,德琪医药有限公司(简称“德琪医药”)宣布,美国国家综合癌症网络(NCCN?)在最新版多发性骨髓瘤临床实践威廉亚洲博彩公司 (NCCN Guidelines?)中添加了三种selinexor(ATG-010)用于治疗复发难治性多发性骨髓瘤(rrMM)患者的组合方案,分别为:基于BOSTON研究支持的SVd方案(selinexor+硼替佐米+地塞米松),基于STOMP研究支持的SDd方案(selinexor+达雷妥尤单抗+地塞米松)以及SPd方案(selinexor+泊马度胺+地塞米松),其中,SPd是一种全口服的治疗方案。本次NCCN?威廉亚洲博彩公司 更新只涉及selinexor内容的更新,值得注意的是,SVd方案成为了威廉亚洲博彩公司 的1类推荐方案,这也标志着以selinexor为骨架的治疗方案将为MM患者提供新的治疗选择。
多发性骨髓瘤是一种克隆浆细胞异常增殖的恶性疾病,在很多国家是血液系统第2位常见恶性肿瘤1。rrMM仍然不能治愈,且易复发,而且复发后缺乏标准的治疗方案。随着越来越多的新药应用于临床,如何选择合适的治疗方案也是临床上面临的难题。NCCN威廉亚洲博彩公司 将为rrMM患者的治疗提供重要指导,国内外的血液学专家对此次威廉亚洲博彩公司 的更新也非常关注,并对selinexor进入新版NCCN威廉亚洲博彩公司 给予了高度评价。
中国医学科学院血液病医院邱录贵教授表示:“近期,NCCN多发性骨髓瘤威廉亚洲博彩公司 更新至2021第四版,selinexor的多个方案被写入最新版的推荐威廉亚洲博彩公司 中。其中,selinexor联合硼替佐米、地塞米松每周一次的方案(SVd)已经写入了复发的rrMM患者的一类方案推荐。今年LANCET中发表了SVd应用于既往接受过1-3线治疗后复发rrMM患者的疗效及安全性,研究数据令人鼓舞。selinexor正在中国进行一项联合地塞米松的注册性II期临床实验,目前这个方案的有效性和安全性和美国注册性临床试验类似,也没有新的安全事件发生。随着williamhill asia 对selinexor联合方案的认识不断深入,临床应用经验不断增多,相信selinexor将会给rrMM患者带来更多的生存希望。”
上海长征医院傅卫军教授表示:“12月10号,NCCN的最新MM威廉亚洲博彩公司 新增了治疗方案,为rrMM患者的治疗提供了更多选择。其中,williamhill asia 也看到了一个熟悉的药物selinexor,这个产品的数据近期相继在血液瘤领域的重要会议上发表。从以往发表的数据看到,SVd治疗既往接受过1-3线治疗后复发的rrMM患者,总有效率(ORR)达76%;SPd治疗多次复发的rrMM患者,ORR接近60%,疗效显着。此外,selinexor联合达雷妥尤单抗治疗方案能够很好地改善整体疗效。研究恰如其分地说明了selinexor作为一种全新作用机制的药物,跟现有药物进行有效组合,能进一步提高疗效,延长患者的无进展生存期。我希望未来能看到更多selinexor联合方案在中国患者中的临床数据,并基于其突出的疗效早日写入中国推荐威廉亚洲博彩公司 ,使更多MM患者获益。“ 德琪医药创始人,董事长兼首席执行官梅建明博士表示:“selinexor进入NCCN推荐威廉亚洲博彩公司 ,是基于该产品治疗复发难治性多发性骨髓瘤的显着疗效;是基于选择性核输出抑制剂应用于肿瘤治疗的可及性和发展潜力;更是基于这一全新机制的口服药物能够切实匹配患者的临床需求。williamhill asia 很荣幸看到selinexor受到专业人士、专业协会的一致认可,williamhill asia 将继续探索该药物的临床应用潜力,让中国、亚太乃至全球患者的受益最大化” 。NCCN威廉亚洲博彩公司 目前是指导全球医疗专家的最佳治疗威廉亚洲博彩公司 ,三种不同的selinexor联合方案进入该威廉亚洲博彩公司 ,进一步验证了selinexor在未来多发性骨髓瘤治疗中的重要性。
关于Selinexor (ATG-010, XPOVIO)
Selinexor (ATG-010, XPOVIO)是同类首款且同类唯一一款口服型选择性核输出抑制剂(SINE)化合物,由德琪医药与Karyopharm Therapeutics Inc.合作研发。2019年7月,美国食品药品监督管理局(FDA)批准selinexor联合低剂量地塞米松用于治疗复发难治性多发性骨髓瘤(rrMM)患者。2020年6月,美国FDA再次批准selinexor作为单药口服疗法用于治疗复发难治性弥漫性大B细胞淋巴瘤(rrDLBCL)患者。selinexor是目前首款且唯一一款被美国FDA批准的口服SINE化合物。此外,selinexor针对多个实体肿瘤适应症开展了多项中期和后期临床试验,包括脂肪肉瘤和子宫内膜癌。2020年11月,德琪医药合作伙伴Karyopharm在2020年结缔组织肿瘤学年会(CTOS 2020)上报告了III期SEAL研究的积极数据,SEAL研究是一项随机、双盲、安慰剂对照交叉研究,旨在比较口服单药selinexor与安慰剂在脂肪肉瘤患者中的疗效。Karyopharm近期公布了selinexor用于治疗子宫内膜癌患者的III期SIENDO研究已通过计划的中期无效性分析。同时,数据安全监查委员会(DSMB)推荐SIENDO研究无需作任何修改按计划继续进行,SIENDO试验的顶线数据预计在2021年下半年公布。 德琪医药正在中国进行selinexor针对复发难治性多发性骨髓瘤的II期注册性临床研究(代号MARCH)以及针对复发难治性弥漫性大B细胞淋巴瘤II期注册性临床研究(代号SEARCH)。同时,德琪医药针对亚太高发瘤种启动了selinexor用于治疗外周T细胞淋巴瘤、NK/T细胞淋巴瘤(代号TOUCH)及KRAS突变的非小细胞肺癌的临床研究(代号TRUMP)。
关于德琪医药
德琪医药有限公司(简称“德琪医药”)是一家专注于创新抗肿瘤药物的亚太地区临床阶段生物制药公司,旨在为中国、亚太地区及全球各地的患者提供最前沿的抗肿瘤创新疗法。自成立以来,德琪医药已建立起拥有12款临床及临床前创新药物的丰富产品管线,取得10个临床批件,并在亚太地区开展10项跨区域临床试验。德琪人以“医者无疆,创新永续”为愿景,力争通过对同类首款/同类最优疗法的专研与市场化,解决亚太乃至全球患者未满足的临床需求。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#治疗方案#
69
#多发性#
0
#新作用#
63
优秀
130
#NCCN#
92
#selinexor#
73
不错
100
学习了
114
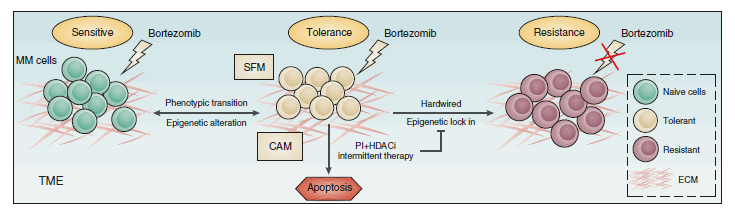
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
94