JAMA Psychiatry:心理干预联合减量药物治疗策略用于抑郁症复发预防
2021-05-25 MedSci原创 MedSci原创
对于药物治疗后症状缓解的抑郁症患者,可采用减少抗抑郁药物的同时接受心理干预的复发预防策略,其效果与持续药物治疗相当

抑郁患者临床复发率较高,首次抑郁后约半数以上患者会在未来的5年以内再次复发。对于复发高风险人群,持续的抗抑郁药物治疗是必须的。临床威廉亚洲博彩公司 建议,对于复发高风险人群,在症状得到缓解后应进行至少为期2年的药物维持治疗。长期的抗抑郁药物治疗带来的副作用显而易见,近年来,心理干预(如预防性认知治疗,正念认知治疗)在预防抑郁复发方面得到广泛应用。近日,研究人员考察了在抗抑郁药物减量期进行心理干预对患者复发风险的影响。
本次研究为系统综述及荟萃分析研究,收集截至2021年1月发表在PubMed、Cochrane图书馆、Embase和PsycInfo等数据库中的相关研究,参与者在接受标准抗抑郁药物治疗后,症状完全或部分缓解,随后继续接受药物维持治疗或减少抗抑郁药物的同时进行心理干预。研究的主要终点为抑郁症复发时间。
本次研究包含4个临床对照研究,714名参与者数据,患者平均年龄49.2岁,女性占73.1%。荟萃分析发现,逐渐减少抗抑郁药物治疗期间进行心理干预vs单独使用抗抑郁药物维持治疗相比,抑郁症复发的时间没有显著差异(危险比[HR]=0.86)。发病年龄较轻(HR=0.98)、缓解期短(HR=0.99)、基线时较高的残留抑郁症状水平(HR=1.07)与总复发风险增加相关。
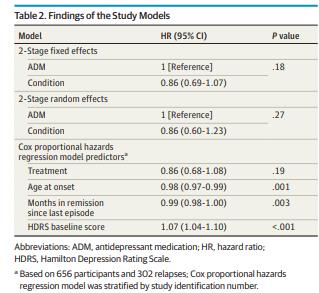
复发风险因素研究
研究认为,对于药物治疗后症状缓解的抑郁症患者,可采用减少抗抑郁药物的同时接受心理干预的复发预防策略,其效果与持续药物治疗相当。
原始出处:
Josefien J. F. Breedvelt et al. Continuation of Antidepressants vs Sequential Psychological Interventions to Prevent Relapse in Depression An Individual Participant Data Meta-analysis. JAMA Psychiatry. May 19, 2021.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#Psychiatry#
61
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
91
棒
114
正在学习中
117
嗯
98
很好
105
受用
63