Sci Transl Med:复发性A型链球菌扁桃体炎是一种免疫敏感性疾病
2019-02-11 AlexYang MedSci原创
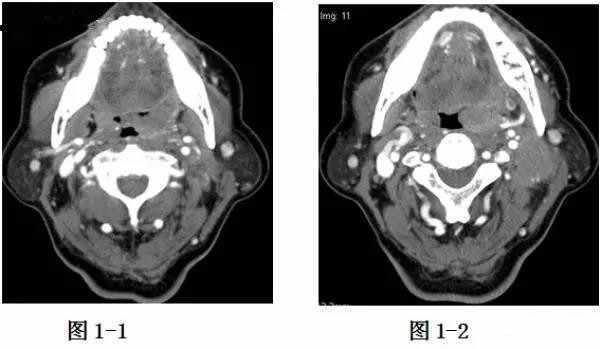
脓毒性咽喉炎在儿童中高度流行,但是为什么仅在某些儿童中发展为复发性扁桃体炎(RT)仍旧不清楚。最近,有研究人员为了进一步认识该经典的儿童疾病,对2个独立的群体-小儿A型链球菌(GAS)RT和非RT扁桃体进行了表型、基因型和功能性研究。研究发现,GAS RT扁桃体具有更小的生发中心,且GAS特异性CD4+生发中心T滤泡辅助细胞(GC-TFH)数量不足。RT儿童表现出了对重要的GAS病毒因子链球菌发热
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#复发性#
59
#TRA#
41
#Transl#
40
学习了长知识
82
#敏感性#
46
#Med#
48
#链球菌#
50