DCR:扩大右侧结肠切除术不会降低结肠癌局部区域复发的风险
2022-04-22 xuyihan MedSci原创
右半结肠切除范围,若对盲肠及升结肠癌,应同时切除回肠末端15cm、盲肠、升结肠、横结肠右半部及部分大网膜和胃网膜血管;切断及切除回盲动脉、右结肠动脉、中结肠动脉右支及其伴随的淋巴结。
右侧结肠癌(RSCC)的切除术已经成为结肠癌治疗的标准手术方式,随着时间的推移,手术技术也有了许多改进,使得直肠癌患者的短期和长期疗效都得到了改善。传统的右半结肠切除术(CRHC)是指切除右结肠,结肠癌患者在初次治疗后容易出现局部区域性复发,其总体生存率一般较低。因此,右半结肠扩大切除术是否是促进生存率提高的因素之一,目前仍有争议。本研究的目的是探究与传统方法相比,扩大手术切除结肠系膜的短期和长期结果差异。

这是一项基于前瞻性维护的丹麦结直肠癌组数据库的回顾性研究。主要观察结局指标是接受右侧结肠癌根治性切除术的患者的局部区域复发情况,次要结局指标是术后 30 天并发症。研究人员还研究了远处转移、非计划的术中不良事件以及术后 30 天和 90 天的死亡率。
研究结果显示在 12855 名切除右侧结肠癌的患者中,1151 名接受了扩大的右半结肠切除术。扩大右半结肠切除术的患者是 ASA 评分较低的年轻男性,由结直肠外科医生使用腹腔镜方法进行手术,并且淋巴结数量显着增加。局部区域复发率为 1.1% (136/12,855),常规右半结肠切除术与扩大右半结肠切除术之间没有差异 (OR 1.7 CI 95% 0.63-2.18)。即使在调整了年龄、合并症、腹部和其他协变量后,扩大右半结肠切除术的术后内科并发症也显着增加(OR 1.26 CI 95% 1.01-1.58)。
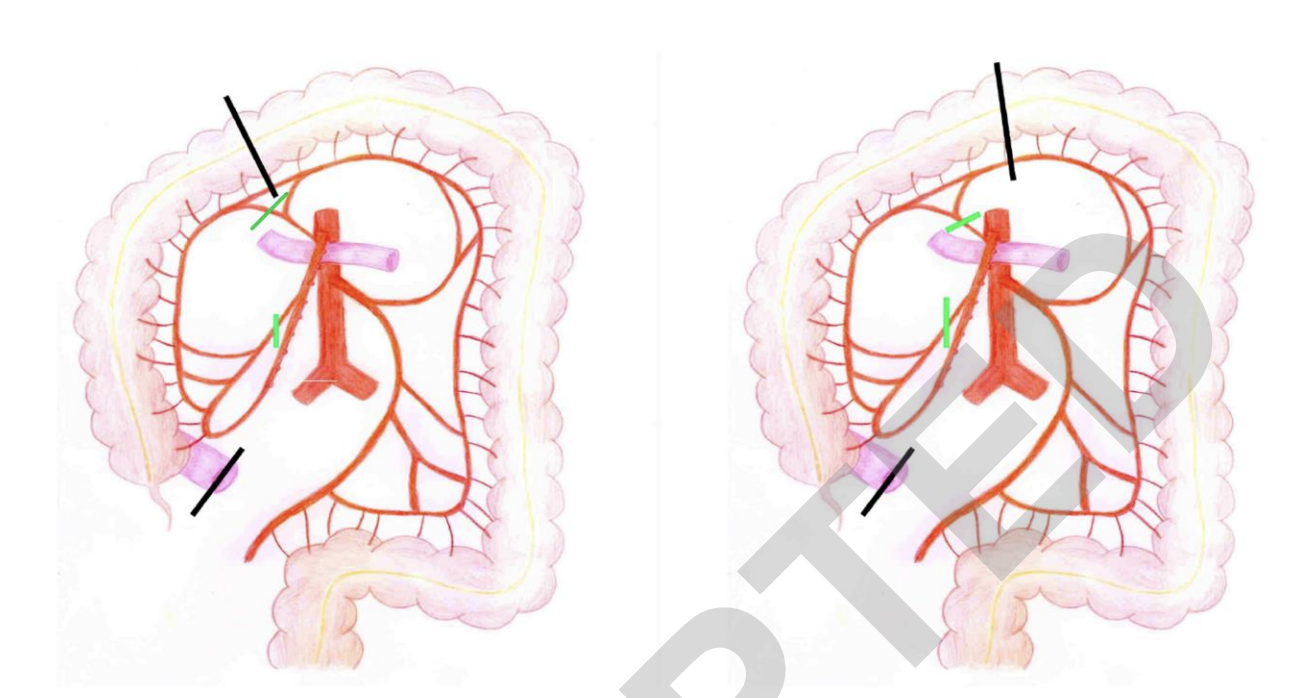
图:手术方式示意图
本项研究表明,在传统的右半结肠切除术和扩大的右半结肠切除术以及肠系膜切除术和中结肠血管结扎术之间,右侧结肠癌的局部区域复发没有差异,但是扩大切除与较高的术后并发症发生率相关。
原始出处:
El-Hussuna, Alaa. Et al. Extended Right-Sided Colon Resection Does Not Reduce the Risk of Colon Cancer Local-Regional Recurrence: Nationwide Population-Based Study from Danish Colorectal Cancer Group Database. Diseases of the Colon & Rectum.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#结肠切除术#
55
#切除术#
54
#局部#
56
好紧张继续继续小惊喜你那
67