J Clin Oncol:埃罗妥珠单抗联合泊马度胺和地塞米松可显著改善复发/难治性多发性骨髓瘤生存预后
2022-08-17 MedSci原创 MedSci原创
在既往接受来那度胺和蛋白酶体抑制剂治疗的复发/难治性多发性骨髓瘤患者中,与泊马度胺/地塞米松相比,埃罗妥珠单抗联合泊马度胺/地塞米松方案具有显著的生存益处
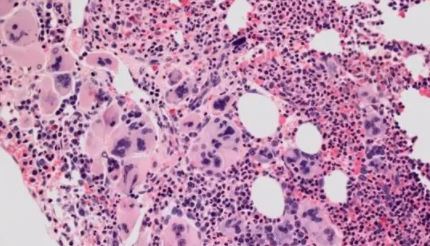
虽然在过去10-15年多发性骨髓瘤 (MM) 疗法取得了显著进步,但 5 年相对生存率仍只有55.6%。在2期ELOQUENT-3试验中,与泊马度胺/地塞米松 (Pd) 相比,埃罗妥珠单抗联合泊马度胺/地塞米松 (EPd) 显著改善了既往接受来那度胺和蛋白酶体抑制剂(PI)治疗过的复发/难治性多发性骨髓瘤 (RRMM) 患者的无进展生存期 (PFS)。本文报告了该试验最终的总生存期(OS)结果。
接受过≥2线治疗的对来那度胺和PI治疗难治性的或复发性的RRMM患者被随机(1:1)分至 EPd 组或 Pd 组。主要终点是无进展生存率(PFS)。次要终点是客观缓解率(ORR)和总生存率(OS)。
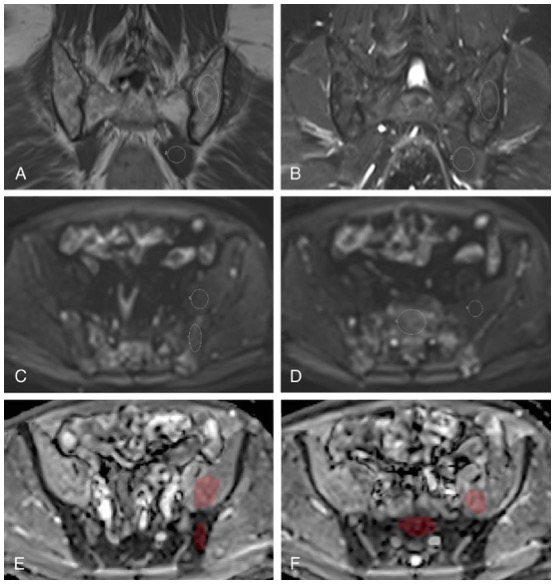
两组的OS
共117位患者被随机分至 EPd 组(n=60)和 Pd组(n=57)。在接受研究治疗的患者中(EPd组 60位,Pd组 55位)。EPd 组和 Pd 组分别有37例(61.7%)和41例(74.5%),大多是因为疾病进展(EPd组 41.7%,Pd组 49.1%)。与Pd组相比,EPd组的中位OS显著延长(29.8个月 vs 17.4个月;HR 0.59,p=0.0217)。在大多数患者亚组中观察到EPd方案带来的 OS 获益。EPd方案的安全概况与既往报告的一致,没有检测到新的安全信号。
总之,在既往接受来那度胺和蛋白酶体抑制剂治疗的复发/难治性多发性骨髓瘤患者中,与泊马度胺/地塞米松相比,埃罗妥珠单抗联合泊马度胺/地塞米松方案具有显著的生存益处。
原始出处:
Meletios A. Dimopoulos, et al. Elotuzumab Plus Pomalidomide and Dexamethasone for Relapsed/Refractory Multiple Myeloma: Final Overall Survival Analysis From the Randomized Phase II ELOQUENT-3 Trial. Journal of Clinical Oncology. August 12, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.02815.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#多发性#
82
#生存预后#
77
#Oncol#
63
#难治性#
76
好文章,值得一读。
75