J Gastroenterology:熊去氧胆酸可以改善原发性硬化性胆管炎患者的长期预后
2022-09-17 xuyihan MedSci原创
PSC是指原发性硬化性胆管炎,主要以肝内外胆管进行性纤维化狭窄等病变为特点的一种自身免疫性疾病,有时病变会进一步蔓延到胰管或者胆囊。
原发性硬化性胆管炎(PSC)是一种病因不明的慢性胆汁淤积性疾病,其特征是由于弥漫性炎症和纤维化导致胆管进行性狭窄和破坏,最终导致肝硬化和肝功能衰竭。尽管这种疾病很严重,但目前还没有标准化的医疗方法。尽管自体免疫反应被认为在 PSC 发病机制中起作用,但免疫抑制剂治疗未能表现出疗效。因此,PSC 患者的长期预后仍然不佳,肝移植 (LT) 是晚期 PSC 患者的唯一选择。熊去氧胆酸 (UDCA)是目前PSC患者使用最多的药物,在现实世界中约有 45-75%的患者使用UDCA。本项研究旨在探究UDCA的使用是否与 PSC 患者的死亡或LT减少显着相关。
研究人员回顾性分析了来自日本PSC登记处的数据,其中包括435名PSC患者。同时研究人员将具有完整诊断数据集的患者纳入本项研究,以及诊断年份、治疗方案、随访期和结果数据。UDCA 治疗与全因死亡或 LT 之间的关联使用 Cox 回归和 UDCA 治疗加权逆概率 (IPTW) 调整的 Cox 回归模型进行协变量调整。
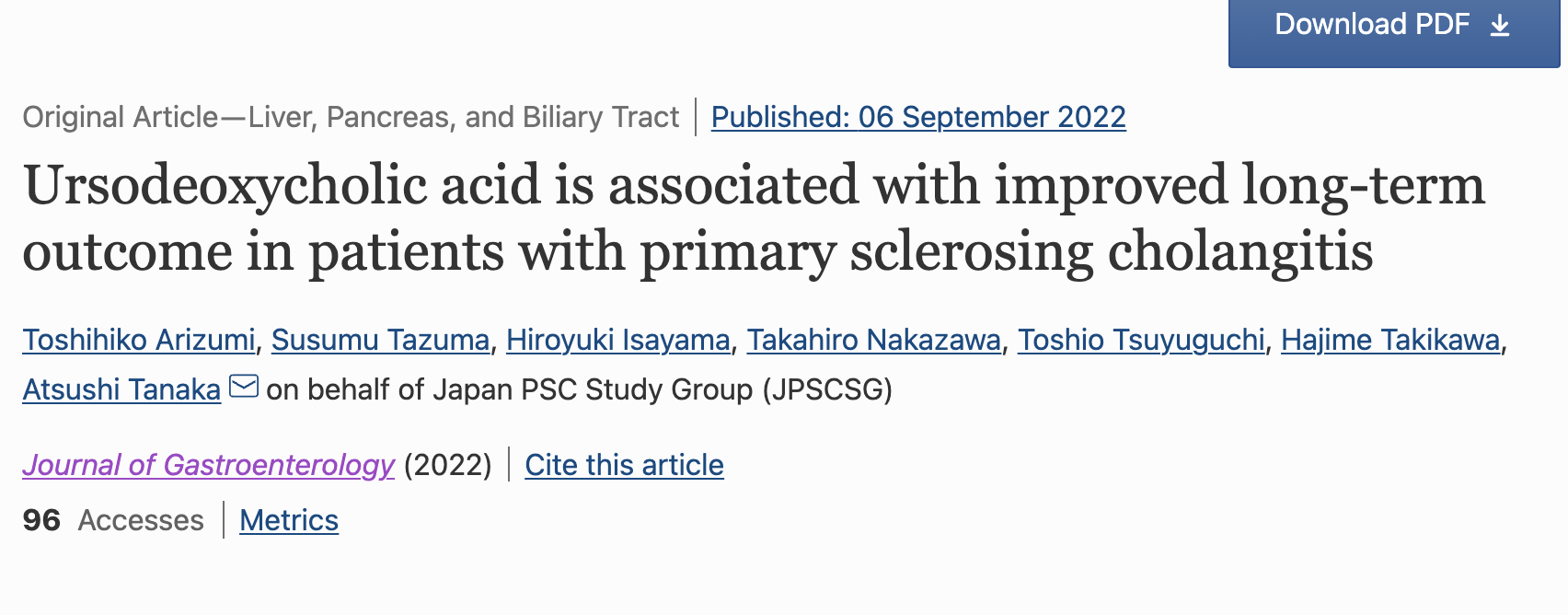
研究结果显示在435名PSC患者中,110名因数据不足或缺失而被排除,其余325名患者(男性,187 人(58%);平均诊断年龄,45.8 岁)被纳入研究。平均随访时间为 5.1 年,观察期间发生 57例患者死亡和24例LT。278 名患者 (86%) 接受了UDCA治疗。Cox 回归模型表明,UDCA治疗与无LT生存期的改善相关[调整后的风险比 (aHR) 0.47, 95% 置信区间 (CI) 0.28–0.78, p=0.003]。此外,IPTW调整模型表明UDCA与无LT生存之间存在显着关联(aHR 0.43, 95% CI 0.25–0.75, p=0.020)。
本项研究证实UDCA的使用与PSC患者无LT生存率的改善显着相关,表明 UDCA 可改善 PSC 患者的长期预后。
原始出处:
Toshihiko Arizumi. et al. Ursodeoxycholic acid is associated with improved long-term outcome in patients with primary sclerosing cholangitis. Journal of Gastroenterology.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#Gastroenterol#
75
#长期预后#
69
#GAS#
71
#原发性#
73
#AST#
66
#原发性硬化性胆管炎#(PSC)是一种病因不明的#慢性胆汁淤积性疾病#,其特征是由于弥漫性#炎症#和#纤维化#导致胆管进行性狭窄和破坏,最终导致#肝硬化#和#肝功能衰竭#。
137
#熊去氧胆酸#
80
#原发性硬化性胆管炎#
87
#硬化性#
62
#Gastroenterology#
62