J Clin Oncol:Durvalumab±Oleclumab/Monalizumab巩固治疗3期非小细胞肺癌的疗效和安全性
2022-04-26 Nebula MedSci原创
与Durvalumab单药治疗相比,两种联合方案均可相对提高客观缓解率和延长无进展生存期
Durvalumab 是一种选择性、高亲和力的人免疫球蛋白 G1 单克隆抗体 (mAb),可阻断程序性细胞死亡配体-1 (PD-L1) 与程序性细胞死亡-1 (PD-1) 和 CD80 的结合,使 T 细胞能够识别并杀死肿瘤细胞。已有研究显示,Durvalumab 显著提高了不可切除的 III 期非小细胞肺癌患者的总体生存率,并且在同步放化疗(cCRT)后无进展。
本研究是一项 II 期研究,目的对比不可切除的 III 期非小细胞肺癌患者在同步放化疗后单独使用 Durvalumab 或联合抗 CD73 单克隆抗体 Oleclumab 或抗 NKG2A 单克隆抗体 Monalizumab 作为巩固治疗的疗效和安全性。
复合纳入标准的患者被随机(1:1:1)分成三组,在 cCRT 后 42 天内接受 Durvalumab 单药或 Durvalumab+Oleclumab 或 Durvalumab+Monalizumab 巩固治疗长达12个月,并按组织学分层。主要终点是调查者判定的客观缓解率(ORR)。
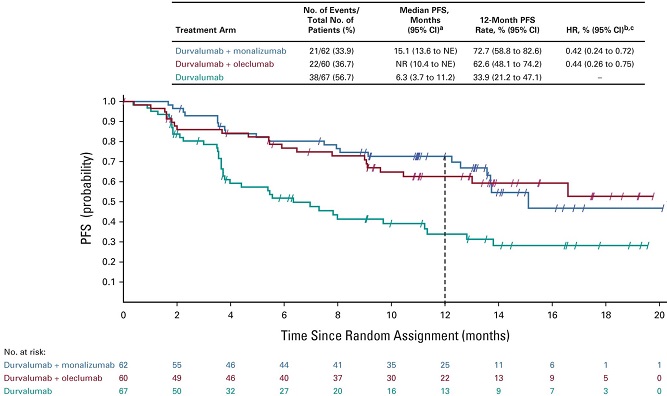
各组的无进展生存率
2019年1月至2020年7月期间,共有189位患者被随机分至三组接受了研究治疗。截止2021年5月17日中期分析时,中位随访了11.5个月。Durvalumab 组、Durvalumab+Oleclumab 组和 Durvalumab+Monalizumab 组的客观缓解率分别是 17.9%、30.0%和35.5%。与 Durvalumab 单药组相比,两个联合治疗组的无进展生存期(PFS)均相对延长(+Oleclumab 组:HR 0.44;+Monalizumab 组:HR 0.42),12个月无进展生存率也更高(Durvalumab 组:33.9%;+Oleclumab 组:62.6%;+Monalizumab 组:72.7%)。
Durvalumab 组、Durvalumab+Oleclumab 组和 Durvalumab+Monalizumab 组的全因≥3级的需紧急治疗的不良反应的发生率分别是39.4%、40.7%和27.9%。
综上,与 Durvalumab单药治疗相比,两种联合方案均可相对提高客观缓解率和延长无进展生存期,且不增加安全性问题。
原始出处:
Roy S. Herbst, et al. COAST: An Open-Label, Phase II, Multidrug Platform Study of Durvalumab Alone or in Combination With Oleclumab or Monalizumab in Patients With Unresectable, Stage III Non–Small-Cell Lung Cancer. J Clin Oncol. https://ascopubs.org/doi/full/10.1200/JCO.22.00227
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#非小细胞#
79
#Oncol#
73
#疗效和安全性#
79
#mAb#
59