JAMA:体外二氧化碳去除促进极低潮气量机械通气对急性低氧性呼吸衰竭患者预后的影响
2021-09-01 MedSci原创 MedSci原创
在急性低氧性呼吸衰竭患者中,与传统的低潮气量机械通气相比,使用体外二氧化碳去除促进极低潮气量机械通气不能降低患者90天死亡率

急性低氧血性呼吸衰竭是ICU入院的主要原因之一,患者死亡和长期并发症风险高,治疗消耗大量的卫生保健资源。有相当大比例的急性低氧血症性呼吸衰竭患者符合急性呼吸窘迫综合征(ARD)的诊断标准,需进行侵入性机械通气以维持足够的气体交换,但由于肺过度充气和损伤,患者预后普遍较差,特别是侵入性机械通气后患者死亡率未见显著降低。"通气与肺保护策略"通过降低潮气量,可改善急性低氧血性呼吸衰竭和ARD患者预后,是少数可降低患者死亡率的干预措施之一。体外气体交换,包括体外二氧化碳去除(ECCO2R),通过去除累积的二氧化碳,可实现更低潮气量的机械通气。近日研究人员考察了体外二氧化碳清除联合低潮气量机械通气是否能改善急性低氧性呼吸衰竭患者的预后。
本次研究在英国51个ICU中心开展,包含412名因急性低氧性呼吸衰竭接受机械通气的成年患者,患者随机接受至少48小时的体外二氧化碳清除促进的低潮气量通气(n=202)或常规低潮气量通气(n=210)。研究的主要终点为90天全因死亡率,次要结果包括第28天无呼吸机天数和不良事件发生率。
患者平均年龄59岁,143名(35%)女性,405名患者(98%)完成了试验。根据数据监测和道德委员会的建议,试验提前停止。低潮气量通气加体外二氧化碳清除组的90天死亡率为41.5%,而标准护理组为39.5%(风险比1.05;差异,2.0%)。与标准护理组相比,体外二氧化碳清除组的平均无呼吸机天数更少(7.1 vs 9.2天)。体外二氧化碳清除组和标准护理组分别有62名患者(31%)和18名患者(9%)发生严重不良事件,其中体外二氧化碳去除组和对照组分别有9名患者(4.5%)和0名患者(0%)发生颅内出血,体外二氧化碳去除组和对照组分别有6名患者(3.0%)和1名患者(0.5%)发生其他部位出血。总体而言,21名患者发生了22起与研究装置相关的严重不良事件。
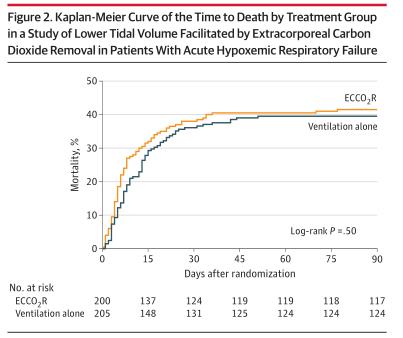
组间90天死亡率差异
研究认为,在急性低氧性呼吸衰竭患者中,与传统的低潮气量机械通气相比,使用体外二氧化碳去除促进极低潮气量机械通气不能降低患者90天死亡率。
原始出处:
James J. McNamee et al. Effect of Lower Tidal Volume Ventilation Facilitated by Extracorporeal Carbon Dioxide Removal vs Standard Care Ventilation on 90-Day Mortality in Patients With Acute Hypoxemic Respiratory Failure The REST Randomized Clinical Trial. JAMA. August 31,2021.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#潮气量#
65
#患者预后#
61
#急性低氧性呼吸衰竭#
69
#二氧化碳#
70
#低潮气量#
62
学习
96
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
85