Lancet:并非所有的免疫治疗都能创造奇迹——帕博利珠单抗未能延长胃/胃食管结合部癌症患者总生存
2018-06-20 biubiugirl 肿瘤威廉亚洲官网
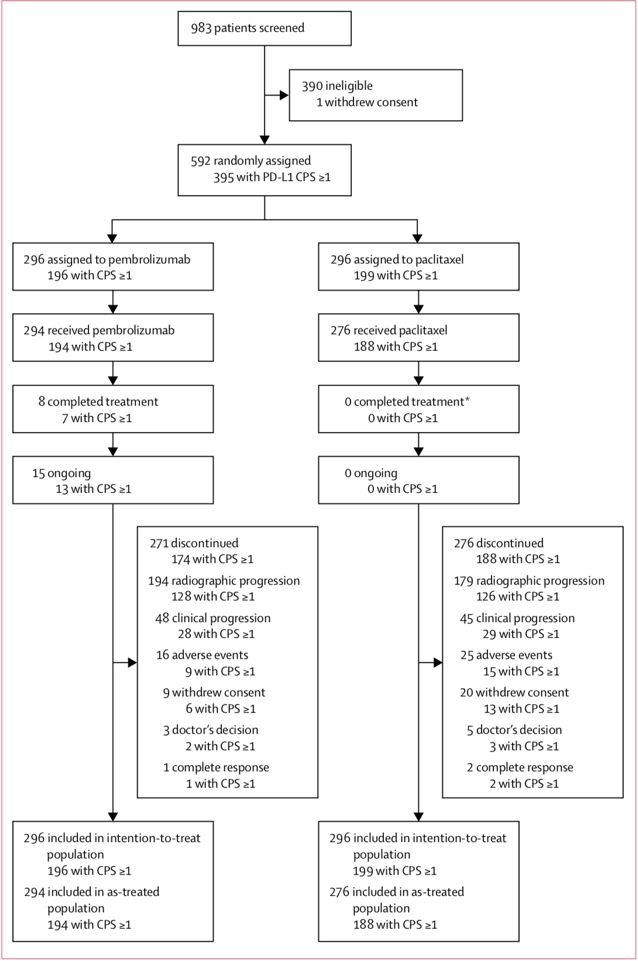
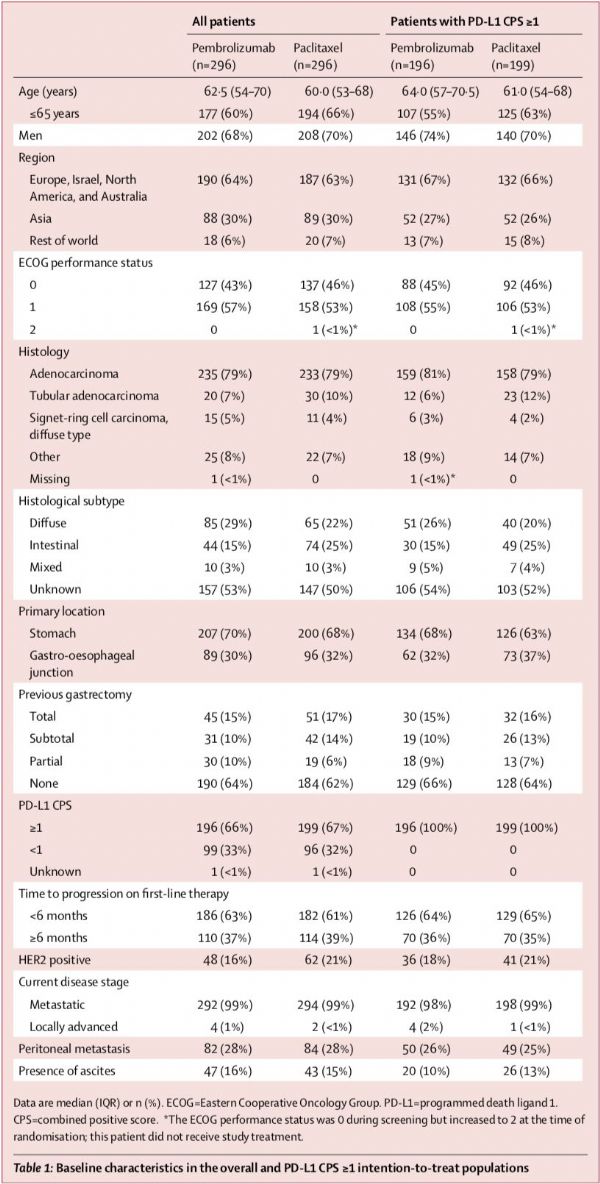
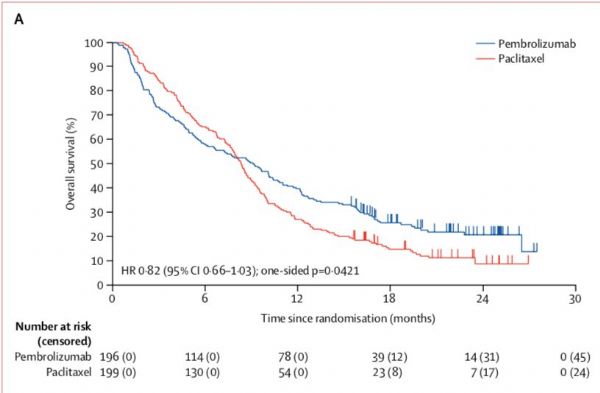
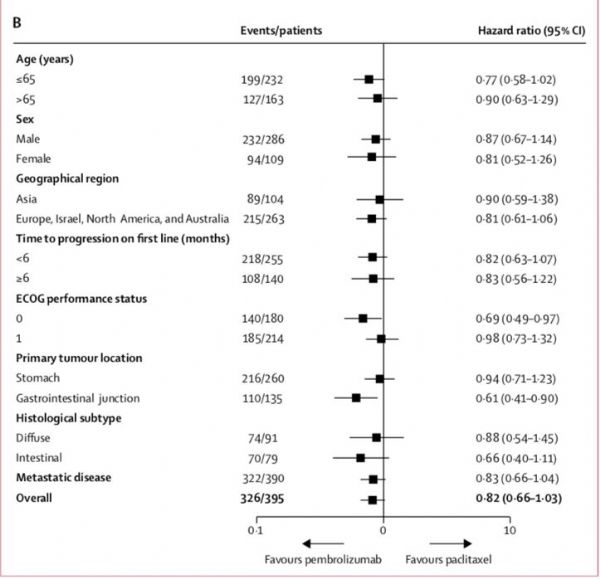
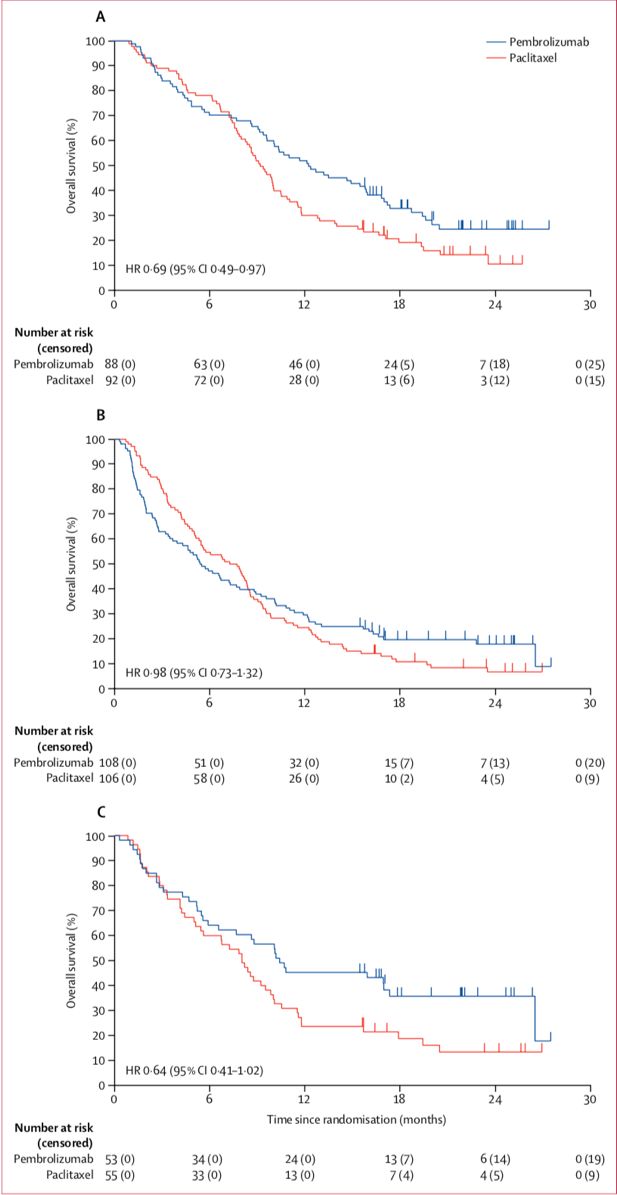
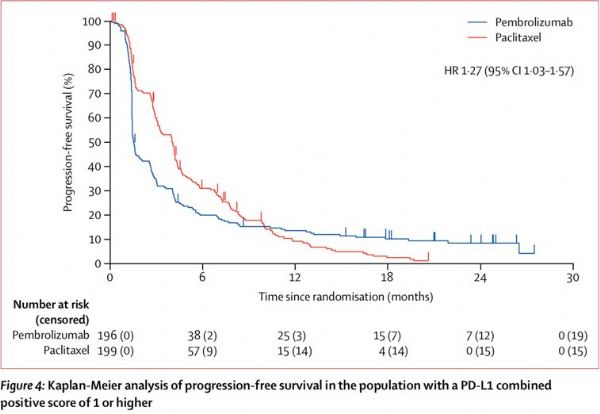
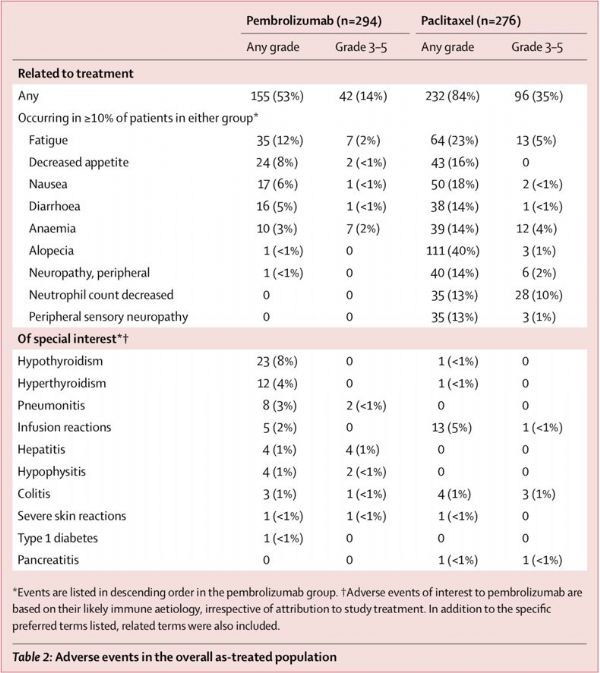
晚期胃癌患者一线治疗后进展者结局通常不佳,而且二线治疗的选择十分有限。但随着免疫检查点阻滞剂的问世,多种肿瘤的治疗模式发生了变化。在晚期胃癌治疗后进展的患者中,免疫检查点阻滞剂是否能同样复制在其他肿瘤中的奇迹呢?KEYNOTE-061研究给了williamhill asia 答案。遗憾的是,即使是在PD-L1联合阳性评分≥1的复发的晚期胃癌或胃食管结合部癌患者中,帕博利珠单抗二线治疗并未能延长其总生存。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#帕博利珠#
51
#Lancet#
53
微卫星不稳定那部分患者是否比化疗效果更好?
91
#胃食管#
52
#癌症患者#
46
#食管#
42
学习学习再学习
104
阅
91
学习了.谢谢分享
82
一起学习学习
83