Rheumatology:抗MDA5+皮肌炎患者RPILD和死亡率风险的时间依赖性变化,中国272例队列研究
2022-08-20 紫菀款冬 MedSci原创
调查抗MDA5+皮肌炎(DM)患者发生快速进展性间质性肺病(RPILD)和死亡的风险是否具有时间依赖性。
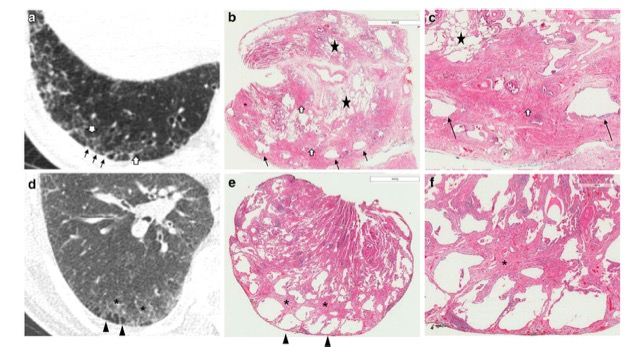
目的:抗黑色素瘤分化相关基因5阳性(抗MDA5+)皮肌炎(DM)与快速进展性间质性肺病(RPILD)密切相关,并与高死亡率相关。然而,关于RPILD的时间依赖性风险和疾病进展期间死亡的数据有限。该研究旨在调查抗MDA5+DM患者发生RPILD和死亡的风险是否具有时间依赖性。

方法:评估了272例抗MDA5+DM患者队列。收集抗MDA5+患者的临床特征,并使用cox回归分析RPILD和死亡的独立危险因素。并描述了RPILD和死亡风险随时间的变化及其潜在的临床意义。
结果:共有272名抗MDA5+DM患者参与该研究。
根据多变量cox回归分析,病程短、CRP水平高、抗Ro52阳性、抗MDA5滴度高( ++~+++)是RPILD的独立危险因素。高CK水平、高CRP水平和RPILD是死亡的独立危险因素。
>90%的RPILD和84%的死亡率发生在发病后的前6个月 。值得注意的是,前3个月是一个特别高风险的时期,发生了50%的RPILD和46%的死亡。在中位随访12年期间,与RPILD和死亡率相关的危险随着时间的推移而减少。
结论:这些结果表明抗MDA5+DM患者的RPILD和死亡率风险存在显著的时间依赖性变化,为估计疾病进展和不良预后提供了一个截止时间窗。
文献来源:
ou H, Wang L, Wang J, et al. Time-dependent changes in RPILD and mortality risk in anti-MDA5+ DM patients: a cohort study of 272 cases in China [published online ahead of print, 2022 Aug 12]. Rheumatology (Oxford). 2022;keac450. doi:10.1093/rheumatology/keac450
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#ILD#
58
#RPI#
67
#Rheumatology#
69
#MDA#
79
#皮肌炎#
71