Cell Rep:浙江大学汪方炜研究组揭示细胞周期的重要调控机制
2018-07-21 佚名 细胞
国际著名学术杂志《Cell》子刊《Cell Reports》杂志在线发表了浙江大学生命科学研究院汪方炜实验室题为“WAC Promotes Polo-like Kinase 1 Activation for Timely Mitotic Entry”的研究论文,揭示细胞周期的重要调控机制。汪方炜实验室的博士生戚菲菲是本文的第一作者,汪方炜教授为通讯作者。

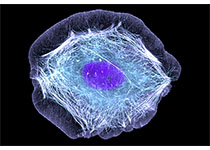
WAC促进细胞核内Plk1激活的分子机制
作为生物繁育和生长发育的基础,细胞增殖最直观的表现是细胞分裂,即由一个亲代细胞变为两个子代细胞,使细胞的数量成倍增加。单细胞生物(如酵母)要保持物种的存在,必须依赖大量的细胞增殖,增加个体数量。多细胞生物则是由一个单细胞即受精卵经过无数次的分裂发育而来。成体生物仍然需要细胞增殖,以弥补代谢过程中的细胞损失。就williamhill asia 人体而言,每天都会有大量的细胞衰老死亡,如皮肤细胞、血细胞、肠上皮细胞等。要维持细胞数量的平衡和机体的正常功能,必须依赖细胞增殖。另外,机体创伤愈合、组织再生、病理组织修复等,也都要依赖细胞增殖。细胞增殖的过程也称为细胞周期,它是一个高度受控、周而复始的连续过程。在高等生物中,细胞周期调控十分复杂,不仅要遵循细胞自身的增殖调控规律,同时还要服从生物体整体的调控。不受约束而生成的细胞可能会转化为癌细胞,最终导致个体的死亡。
一个细胞周期可以简单地划分为两个相互延续的时期,即细胞分裂期(M期)和居于两次分裂期之间的分裂间期,分裂间期是细胞增殖的物质准备和积累阶段,分裂期则是细胞增殖的实施过程。在一个标准的细胞周期中,分裂间期由G1期、S期和G2期先后连续的三个时相组成。G1期是细胞周期的第一阶段,上一次细胞分裂之后,产生两个子代细胞,标志着G1期的开始。S期即DNA合成期,DNA复制完成以后,细胞即进入G2期。只有当所有利于细胞分裂的因素得以满足以后,细胞才能顺利实现从G2期向M期的转换。细胞周期中各个时相的有序更迭和整个细胞周期的运行,需要“引擎”分子的驱动,即是在周期蛋白(Cyclin)依赖的蛋白激酶(Cyclin-dependent kinase, Cdk)统一调控下进行的。不同的Cyclin在细胞周期中表达的时期不同,并与不同的Cdk结合,形成不同种类的Cyclin-Cdk激酶复合物,调节不同的Cdk活性,从而驱动细胞周期的有序运行。
细胞从分裂间期的G2期进入到分裂期(即G2/M期转换)依赖于Cyclin B1-Cdk1激酶复合物的活性。在G2的早期,与Cyclin B1结合的Cdk1被Wee1及Myt1激酶磷酸化,导致活性的抑制。只有当蛋白磷酸酶Cdc25去除Wee1及Myt1对Cdk1的磷酸化后,Cyclin B1-Cdk1才能被激活,进而促成G2/M期转换。Cdc25的活性则依赖于蛋白激酶Plk1对其的磷酸化。因此,G2期Plk1的及时激活对于Cyclin B1-Cdk1活性的激发以及G2/M期的转换极其重要。
汪方炜实验室研究发现,WAC蛋白(全称WW domain-containing adaptor protein with a coiled-coil region)具有多个高度保守的S-S/T-P基序。在G2早期的细胞核内,Cyclin A2-Cdk1激酶复合物磷酸化WAC蛋白的这些S-S/T-P基序。利用RNA干扰技术敲减WAC的表达,会导致细胞周期在G2/M期转换的延缓,回补外源的野生型WAC可以恢复正常的G2/M期转换,而不能被Cyclin A2-Cdk1磷酸化的WAC突变体则不具备这个能力。
进一步研究发现,Cyclin A2-Cdk1对WAC的S-S/T-P基序的磷酸化使其结合Plk1的Polo盒结构域(Polo-box domain, PBD)。敲减WAC的表达或通过突变S-S/T-P基序破坏WAC与Plk1-PBD的结合,则会导致Plk1激酶活性的下降(主要指标是Aurora-A激酶对Plk1激酶域第210位苏氨酸的磷酸化的下调)。
细胞裂解液的免疫共沉淀实验显示,WAC与Aurora-A及Plk1以复合物的形式存在于G2期的细胞中。GST pulldown等实验结果显示,纯化的WAC蛋白能直接结合Aurora-A激酶。在体外磷酸化实验中,被Cyclin A2-Cdk1磷酸化的WAC蛋白能够显着增强Aurora-A对Plk1的磷酸化,而未经预磷酸化处理或不能结合Plk1的WAC突变体则没有这个能力。
上述实验结果表明,在细胞周期的G2期,通过结合Aurora-A及Plk1,WAC蛋白促成Aurora-A对Plk1的磷酸化,进而激发细胞核内Plk1的活性。充分激活后的Plk1可以通过磷酸化Cdc25等途径激发Cyclin B1-Cdk1的活性,从而确保G2/M期的顺利转换和细胞的正常增殖。激活后的Cyclin B1-Cdk1可以类似的方式磷酸化WAC的S-S/T-P基序,在细胞进入分裂期Cyclin A2被降解后继续维持WAC与Plk1的结合以及Plk1的活性。
这项研究不仅鉴定了一个新的Plk1结合蛋白WAC,揭示了其在激活Plk1中的重要作用,而且阐明了调控G2/M期转换的关键机制,对于深入理解细胞周期调控的分子机理,以及Cdk1和Plk1靶向的抗癌药物研发具有重要意义。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#Cell#
51
#CEL#
42
#浙江大学#
59
#细胞周期#
41
#调控机制#
46
这样的研究好厉害
67
好厉害!
83
学习一下
90