双侧延髓内侧梗死继发单侧肥大性下橄榄核变性一例
2020-01-15 杨书祥 赵璐 高远 中华神经科杂志 神经科病例撷英拾粹
延髓内侧梗死是少见的脑血管病,多由脊髓前动脉或椎动脉病变造成。双侧延髓内侧梗死更为少见。肥大性下橄榄核变性(hypertrophic olivary degeneration,HOD)是一种特殊的跨突触变性,多出现在Guillain-Mollaret三角受到损伤之后的一段时间。目前关于延髓病变继发HOD的报道较少,国内尚未见相关报道,延髓病变与HOD之间的关系也没有明确的描述。现就1例双侧延髓内侧
延髓内侧梗死是少见的脑血管病,多由脊髓前动脉或椎动脉病变造成。双侧延髓内侧梗死更为少见。肥大性下橄榄核变性(hypertrophic olivary degeneration,HOD)是一种特殊的跨突触变性,多出现在Guillain-Mollaret三角受到损伤之后的一段时间。目前关于延髓病变继发HOD的报道较少,国内尚未见相关报道,延髓病变与HOD之间的关系也没有明确的描述。现就1例双侧延髓内侧梗死继发单侧HOD患者的临床特点和诊疗经过进行分析,以增加临床对该病的认识。
临床资料
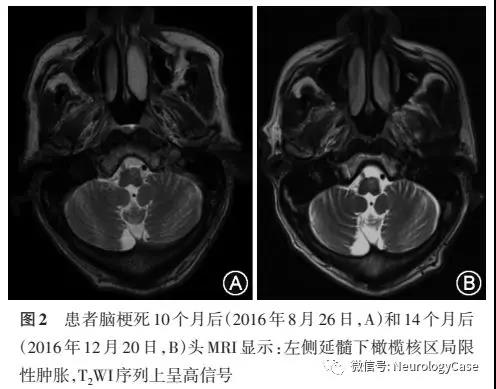
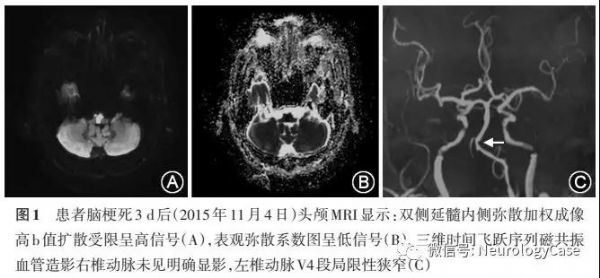
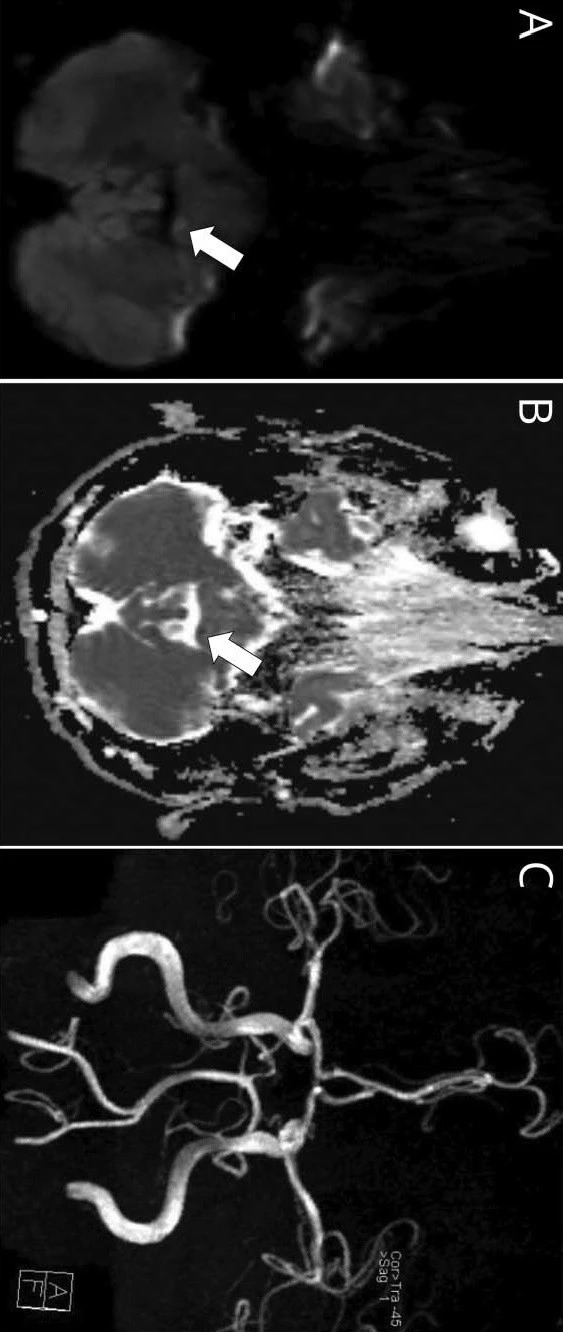
患者男性,66岁,以“脑梗死后头晕1年半,加重伴行走不能半年余”为主诉于2017年4月19日入郑州大学第一附属医院神经内科。1年半前,患者以“右侧肢体无力12h”为主诉于2015年11月1日入我院急诊科,该次入院12 h前突然出现右侧肢体麻木无力,伴头晕,未诊治;入院6h前右侧肢体无力症状加重,且出现言语不清、口角歪斜。查头颅MRI(2015年11月1日)示延髓急性脑梗死,双侧延髓内侧弥散加权成像(DWI)高b值扩散受限呈稍高信号,表观弥散系数(ADC)图上呈低信号,T1WI、T2WI 和T2 FLAIR未见显影。按急性脑梗死治疗,后病情加重,出现头晕、恶心、呕吐、呃逆、嗜睡、呼吸无力及左侧肢体无力,转入重症监护病房治疗,发病3d后复查头MRI(2015年11月4日):双侧延髓内侧病变呈稍长T1长T2信号,T2 FLAIR序列上呈高信号,DWI高b值扩散受限呈明显高信号,ADC图呈低信号,左侧病变较右侧明显(图1)。经治疗后病情好转,肢体无力恢复,仍遗留头晕,呈持续性,非眩晕,走路有不稳感,可不借助工具独立行走。本次就诊半年前,头晕逐渐加重,走路时明显,无恶心、呕吐、耳鸣,不能独自行走及站立,需借助拐杖及在别人的帮助下行走。出院后分别于 2016年8月26日因“冠心病”入我院老年心血管科,2016年12月16 日因“糖尿病”入我院老年内分泌科,住院期间复查头MRI显示左侧延髓下橄榄核区局限性肿胀(图2)。因症状逐渐加重,再次就诊于我院神经内科。既往“高血压病”20余年,血压最高达210/115mmHg(1mmHg=0.133kPa),间断服用降压药物,血压控制在140/90mmHg;“糖尿病”12年,口服“消渴丸”,血糖控制具体不详。
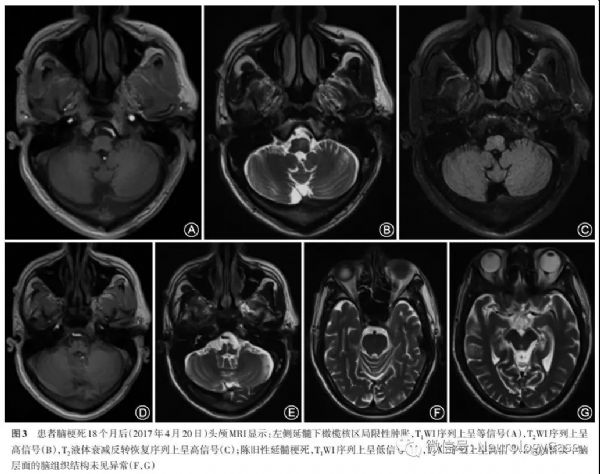
本次入院神经系统体格检查:患者意识清楚,体检配合,吟诗样言语,双眼自发性跷跷板样眼震,眼震粗大,右眼眼震垂直方向向上,左眼眼震垂直方向向下,双眼眼震有顺时针扭转的成分,向各个方向凝视时眼震方向改变,偶有饮水呛咳,洼田饮水试验2级,悬雍垂居中,双侧软腭上抬有力,咽反射存在,无腭肌阵挛,伸舌右偏。右下肢肌力V-级,轻瘫试验阳性,余肢体肌力V级,四肢肌张力稍增高,双侧巴宾斯基征阳性,平衡障碍明显,不能独自站立或行走,双手指鼻不准、轮替动作慢,双下肢跟膝胫试验不稳,右侧明显,肢体无震颤,右下肢深感觉减退,浅感觉检查无异常。本次入院后再次查头颅MRI(2017年4月20日):陈旧性延髓梗死,左侧延髓下橄榄核区局限性肿胀伴等T1长T2信号,T2 FLAIR 序列上呈高信号,头颅磁敏感加权成像未见异常(图3)。
入院期间应用加巴喷丁胶囊、改善循环、营养神经药物及康复治疗,患者自觉头晕症状稍有改善,行走不稳无改善,体征较入院时无改善。出院1年后,对该患者进行随访,患者症状和体征无明显变化。
讨论
HOD是原发病灶累及Guillain-Mollaret三角后出现的跨突触变性,常见的病因有海绵状血管瘤、手术、出血、梗死、肿瘤、外伤、炎症、脱髓鞘、变性疾病及放射性损伤等。原发病灶常位于中脑、脑桥或小脑。脑梗死是HOD 的常见病因,也是我国最常见的脑卒中类型,占脑卒中的69.6%-70.8%。本例患者的梗死灶位于延髓,延髓内侧梗死仅占所有脑梗死的0.5%-1.5%,而继发HOD的病例更为少见。目前的报道中,继发于延髓的HOD极为少见,国际上目前仅有3例延髓病变继发HOD的报道,国内尚未见相关报道。Leestma和Noronha于1976年报道1例左侧延髓内侧梗死继发HOD的病例,病理结果显示左侧延髓上部内侧梗死及左侧下橄榄核肥大;Inoue等于2014年报道了1例双侧延髓内侧梗死之后继发双侧HOD及全延髓水肿的病例;Smets等描述了1例临床表现为持续性腭肌阵挛,头MRI显示为延髓中线海绵状血管瘤引起的双侧HOD。
完整的Guillain-Mollaret三角由一侧齿状核、对侧红核和对侧下橄榄核组成。齿状核的神经纤维经小脑上脚,交叉后到达对侧红核,红核发出的神经纤维经中央被盖束到达同侧的下橄榄核,下橄榄核再发出神经纤维经小脑下脚到达对侧小脑皮质,继而投射到小脑齿状核。williamhill asia
在本例患者的MRI上可以观察到原发病变位于延髓上部(图1),梗死灶平面在下橄榄核平面之上且左侧更为严重,累及双侧锥体束及左侧中线旁结构,头MRI及SWI未见其他累及Guillain-Mollaret三角的病变。推测延髓左侧中线旁梗死损伤到了左侧中央被盖束终止于下橄榄核之前的部位,从而导致左侧HOD。
HOD最核心的临床特点包括:Guillain-Mollaret三角上的原发病变、迟发性特征性症状(如腭肌阵挛、眼震、复视、共济失调、肢体阵挛等)、下橄榄核增大且T2WI序列上呈高信号。当Guillain-Mollaret三角受损之后,下橄榄核的神经元失去了上游神经元的抑制从而出现异常活动,患者常表现出腭肌阵挛、眼震、复视、共济失调、肢体阵挛等特征性症状。本例患者在急性延髓梗死病情好转稳定1年后,出现了新发的进行性加重的症状,以眼震和共济失调为主要特征,但是并没有表现出腭肌阵挛,头MRI显示左侧延髓下橄榄核区局限性肿胀及T2WI 序列上呈高信号。腭肌阵挛是HOD的代表性体征,但并非出现在所有病例中,Onen等的报道显示20%-45%的患者表现出这一体征。
HOD的MRI特点是延髓下橄榄核区局限性T2WI序列高信号。本例患者延髓梗死后10个月的MRI可见左侧下橄榄核增大,T2WI序列上下橄榄核区高信号,病变在延髓梗死后18个月持续存在。据文献统计,原发损伤出现后前3个星期下橄榄核区通常没有异常表现,损伤出现后从第4个星期一直到第4年均可以观察到T2WI序列高信号。下橄榄核体积增大发生在损伤出现后第6个月到第4年,3-4年后下橄榄核逐渐萎缩,T2WI序列上高信号仍然持续。本例患者在我院住院之前曾2次复查头颅MRI,回顾资料发现,复查时已经有临床症状和影像学改变出现,但当时并未诊断HOD且影像学报告并未提示,考虑与以下因素有关:首先,延髓病变继发HOD少见,临床医生及影像科医生对此疾病缺乏认识;其次,原发的延髓病灶和继发的HOD病灶在影像学上结构毗邻,造成容易漏诊。
目前,HOD无特效治疗药物,虽有报道显示加巴喷丁及美金刚可改善HOD 患者的眼震,但其疗效未得到公认。本例患者应用加巴喷丁,仅有主观头晕的稍微改善,眼震及行走不稳无改善。
williamhill asia
报道的是1例罕见的病例,在临床工作中需要提高对该病的认识。当患者既往有Guillain-Mollaret三角的病变时,要考虑到 HOD 的可能,应提高认识,避免漏诊及误诊。
原始出处:
杨书祥,赵璐,刘浩,等.双侧延髓内侧梗死继发单侧肥大性下橄榄核变性一例.《中华神经科杂志》2019年11期
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#肥大性下橄榄核变性#
0
#继发#
46
#延髓#
66
#肥大性#
73
#变性#
49
#双侧#
64