cancer cell:新发现:高可塑性细胞状态揭示了癌细胞的耐药性机制
2020-07-28 Lauren 转化医学网
导言:众所周知,药物治疗癌症已经成为重要的治疗手段,近些年来,各种新型的抗癌新药层出不穷,也取得了一定的治疗效果。然而许多的抗癌药物在开始使用时效果往往不错,但经过一段时间之后逐渐变得疗效不佳或甚至无
导言:众所周知,药物治疗癌症已经成为重要的治疗手段,近些年来,各种新型的抗癌新药层出不穷,也取得了一定的治疗效果。然而许多的抗癌药物在开始使用时效果往往不错,但经过一段时间之后逐渐变得疗效不佳或甚至无效,这也是人们常常所说的肿瘤出现耐药性了。
长期以来,癌症对化疗产生耐药性一直是实现其持久缓解或治愈的主要障碍。虽然化疗后肿瘤可能会很快缩小,但很多时候它们最终还是会长回来。
科学家们曾经认为,肿瘤中独特的基因突变是耐药性的基础。但现在他们越来越多地把目光投向癌细胞的其他非基因变化,以解释它们的适应性。例如,癌细胞产生耐药性的一种方式是改变它们的身份。对激素阻断疗法敏感的前列腺癌细胞可能会转变为不需要激素的细胞类型。
不是特定的突变驱动它们,像这样的身份变化是通过基因表达的变化而来的——细胞开启或关闭特定的基因。这些变化的结果是,单个肿瘤的细胞构成会变得非常不同。这种异质性给治疗带来了挑战,因为单一药物不太可能对如此多的不同细胞类型起作用。
最近,来自斯隆凯特林研究所、麻省理工学院科赫研究所综合癌症研究所和布罗德研究所卡拉曼细胞天文台的研究人员组成的研究小组发现,这种肿瘤异质性可以追溯到一个共同的来源:一种特别灵活的细胞状态,这种状态是肿瘤细胞亚群的特征,可以产生许多不同的细胞类型。该研究在7月23日发表在《癌细胞》杂志上。
SKI癌症生物学和遗传学项目的助理成员、该论文的通讯作者Tuomas Tammela表示,“高可塑性的细胞状态是williamhill asia 在肿瘤中看到的大部分异质性的起点,这有点像许多道路的繁忙交叉路口,高可塑性的细胞状态处于中心位置。”
由于这种细胞状态产生了肿瘤中几乎所有的细胞异质性,它是潜在疗法的一个有吸引力的目标。
研究人员检测的特殊肿瘤是在小鼠体内生长的肺癌肿瘤。在Tammela实验室做研究的医学科学家、该论文的主要作者之一Jason Chan表示,“发现这种不寻常的细胞状态是一个惊喜。这种高度可塑性的细胞状态是一种全新的东西。当williamhill asia 看到它的时候,williamhill asia 不知道它是什么,因为它太不一样了。从癌症的来源来看,它不像正常的肺细胞,也不像肺癌。它具有胚胎胚层干细胞、软骨干细胞、甚至肾细胞混合在一起的特征。”

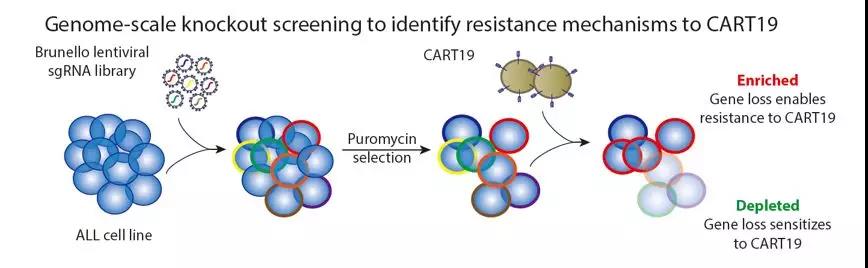
图解摘要
然而,他和他的同事在他们检查的每个肿瘤中都发现了这些细胞,这表明这些细胞在生物学上起着非常重要的作用。
一个细胞呈现的路线图
研究人员通过使用一种相对较新的实验室技术——单细胞RNA测序(scRNA-Seq)来识别这些高度可塑性的细胞。这种技术可以让研究人员对单个细胞的基因表达谱进行“快照”——揭示哪些基因是开启的,那些是关闭的。在肿瘤随着时间的推移变化过程中,使用scRNA-Seq他们能够看到不同的细胞类型何时以及如何出现肿瘤的进化。根据这些数据,研究人员能够绘制出一种图谱,说明哪些细胞来源于哪些细胞。
这种高可塑性的细胞状态在肿瘤的进化过程中始终存在,并在整个肿瘤生长过程中持续存在。事实上,Tammela博士说,“这是williamhill asia 发现的唯一存在于每个肿瘤中的细胞状态。”
不是干细胞
可塑性是细胞分化成具有不同特征的其他细胞的能力,是干细胞的一个众所周知的特征。干细胞在胚胎发育和组织修复中发挥着重要作用。许多科学家认为癌症是由特定的癌症干细胞引起的。
但是Tammela博士和他的同事们并不认为这些高可塑性的细胞是干细胞。当她们将这些高度可塑性细胞的基因表达特征与正常干细胞或已知癌症干细胞进行比较时,这些特征完全不匹配。它们看起来完全不同。与干细胞不同的是,它们在肿瘤生长之初并不存在。它们只是在之后才出现。
改变耐药性
之前的许多研究都在寻找可能的“耐药突变”——一种解释肿瘤抵抗抗癌药物作用能力的基因变化。虽然已经发现了一些耐药性,但更多时候耐药性的基础仍然是个谜。新的发现为这个谜题提供了一个可能的答案。
Chan表示,“williamhill asia 的模型可以解释为什么某些癌细胞会对治疗产生耐药性,而且williamhill asia 不能够识别出这种耐药性的遗传基础。重要的是,并不是肿瘤中的所有细胞都在适应。
研究人员认为,通过结合化疗药物和针对这些高度可塑性细胞的新药物,有可能避免耐药性的出现,并提供更持久的缓解。
原始出处:
Nemanja Despot Marjanovic, Matan Hofree, Jason E. Chan, et.al. Emergence of a High-Plasticity Cell State during Lung Cancer Evolution. Cancer Cell July 23, 2020
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#CEL#
52
#Cell#
49
#cancer cell#
58
#新发现#
54
#癌细胞#
56
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
86