耀斑反应性水凝胶治疗关节炎
2018-04-07MedSciMedSci原创
关节炎症状往往不可预测且常常突然恶化,这些事件使得炎症性关节炎(包括类风湿性关节炎和银屑病关节炎)的处理对患者和医生都极具挑战性
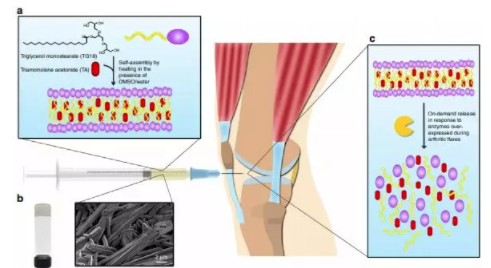
关节炎症状往往不可预测且常常突然恶化,这些事件使得炎症性关节炎(包括类风湿性关节炎和银屑病关节炎)的处理对患者和医生都极具挑战性。但伯明翰妇女医院(BWH)的研究人员发现,耀斑可能也是改善患者治疗方案的重要机会。在实验室进行的研究中,BWH生物工程师开发了一种水凝胶,这是一种柔韧的材料,可以装载关节炎药物并局部注入发炎关节。水凝胶并非以稳定的速率持续输送药物,而是设计用来对疾病的耀斑活动增加作出反应,即当症状恶化时释放药物。该团队的研究结果本周在Nature Communications上发表,研究人员正在努力将这一技术推向临床。
BWH的生物工程师兼首席研究员Jeff Karp博士说,“关节炎代表了巨大的未满足的临床需求,尽管已经开发出新的治疗方法,但许多方案具有全身毒性。williamhill asia 希望设计一种高效的输送系统,可以输送药物并释放药物来应对炎症”。新的耀斑响应性水凝胶由三甘油单硬脂酸酯(TG-18)制成,该化合物是美国食品和药物管理局认定的“公认安全”化合物的一种,TG-18是一种能够自组装的分子,意味着它可以形成包含纤维的凝胶状结构。在本研究中,TG-18水凝胶装载了曲安奈德(TA),但TG-18可能装载多种类型的抗炎化合物。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/74244/flare-responsive-hydrogel-arthritis/
本文系williamhill asia 医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#反应性#
101
#关节炎#
110
#水凝胶#
82
#凝胶#
87