克唑替尼治疗有脑转移的进展期ROS1阳性NSCLC患者的临床疗效结果公布
2017-10-18 佚名 肿瘤威廉亚洲官网
WCLC2017,陆舜教授公布了有脑转移的ROS1阳性患者的治疗效果,结果显示有脑转移的ROS1阳性NSCLC患者能从克唑替尼治疗中显着获益。可喜的是,在同一天,CFDA批准了克唑替尼在ROS1阳性的晚期NSCLC中的适应症。
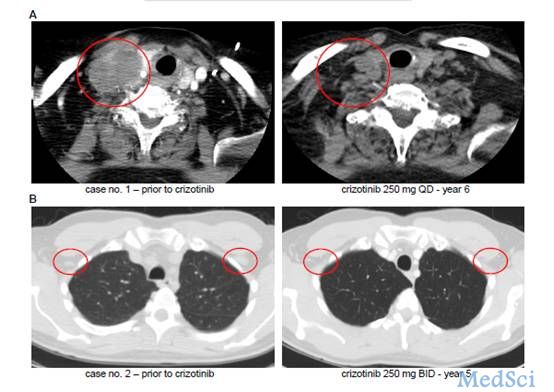
ROS1阳性NSCLC约占所有NSCLC的1-2%左右。对于初诊ROS1阳性晚期NSCLC患者中,大约20%的患者发生脑转移。克唑替尼已经被批准用于用于ALK阳性或者ROS1阳性NSCLC的治疗。大量研究显示,对于伴有脑转移的ALK阳性NSCLC,克唑替尼显示出良好的疗效。而对于伴有脑转移的ROS1阳性NSCLC患者是否能从克唑替尼治疗中显着获益还没有详细的研究报道。
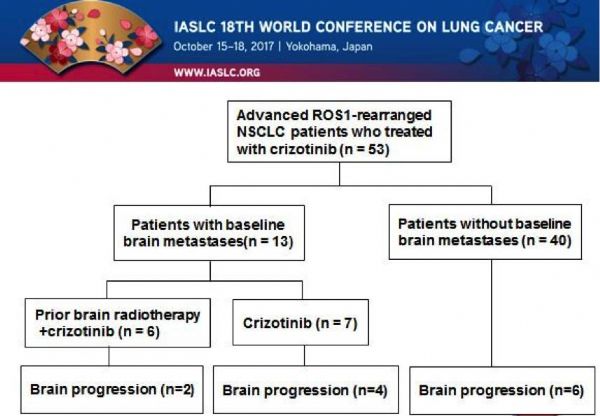
关于这个问题,10月17日,在日本横滨召开的第18届世界肺癌大会上,来自上海胸科医院的陆舜教授公布了他们关于克唑替尼治疗有脑转移的晚期ROS1阳性NSCLC患者疗效的研究成果。该研究主要目的在于了解晚期ROS1阳性NSCLC脑转移的状况,评估克唑替尼治疗ROS1阳性NSCLC患者脑转移的临床疗效。
研究设计
该研究表明,基线无脑转移的患者在接受克唑替尼治疗后,显示出更长的无进展生存期(PFS)以及总生存期(OS)
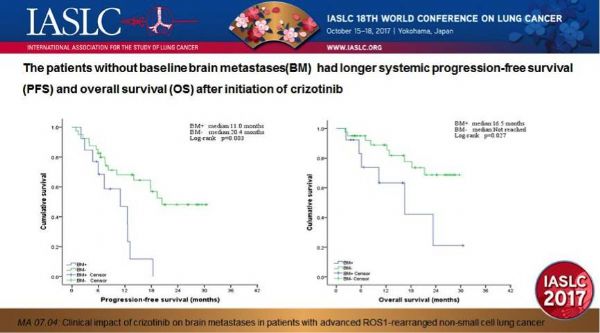
对于基线有脑转移的患者,46.2%的基线脑转移患者既往接受过脑部放疗。在这些患者中,有33.3%的患者在接受克唑替尼治疗前6个月的完成了放疗。在既往接受过脑部放疗与未接受过脑部放疗的患者的颅内无进展生存期(intracranial PFS)无显着差异(中位颅内PFS:12.5个月 vs. 11.0个月,p=0.790)。
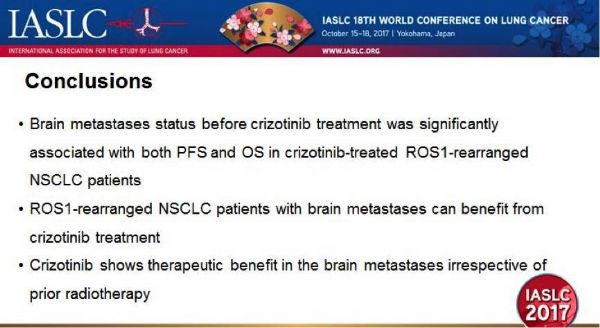
该研究结果表示,在接受克唑替尼治疗前是否存在脑转移与克唑替尼治疗ROS1阳性NSCLC患者的PFS和OS均显着相关。有脑转移的ROS1重排的NSCLC患者能显着从克唑替尼治疗中获益。克唑替尼用于治疗脑转移的效果非常显着,与既往是否有放疗并无相关性。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#ROS1阳性#
77
#进展期#
85
#结果公布#
56
#阳性NSCLC#
84
#临床疗效#
77
#SCLC患者#
78
#ROS#
57
#NSCLC患者#
71
#ROS1#
85