JAHA:流感疫苗对心血管疾病患者死亡率和心血管结局的影响
2021-03-13 MedSci原创 MedSci原创
心血管疾病患者接种流感疫苗以降低死亡率和心血管事件。临床医生和卫生系统应继续推广流感疫苗,作为全面二级预防的一部分。
流行性感冒可在心血管疾病患者中引起相当大的发病率和死亡率。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员评估了流感疫苗对心血管疾病患者死亡率和心血管结局的影响。

研究人员检索了PubMed、Embase和Cochrane图书馆确定了在2020年1月之前发表的评估流感疫苗对心血管疾病患者死亡率和心血管结局影响的随机对照试验和观察性研究。估计值报道了伴有95%CI的随机效应风险比(RRs)。研究人员通过研究设计将随机对照试验和观察性研究进行分层分析。

该研究总共确定了16项研究(n=237058),包含4项随机对照试验(n=1667)和12项观察性研究(n=235391)。参与者的平均年龄为69.2±7.01岁,女性为36.6%,高血压患者占65.1%,糖尿病为31.1%,吸烟者为23.4%。
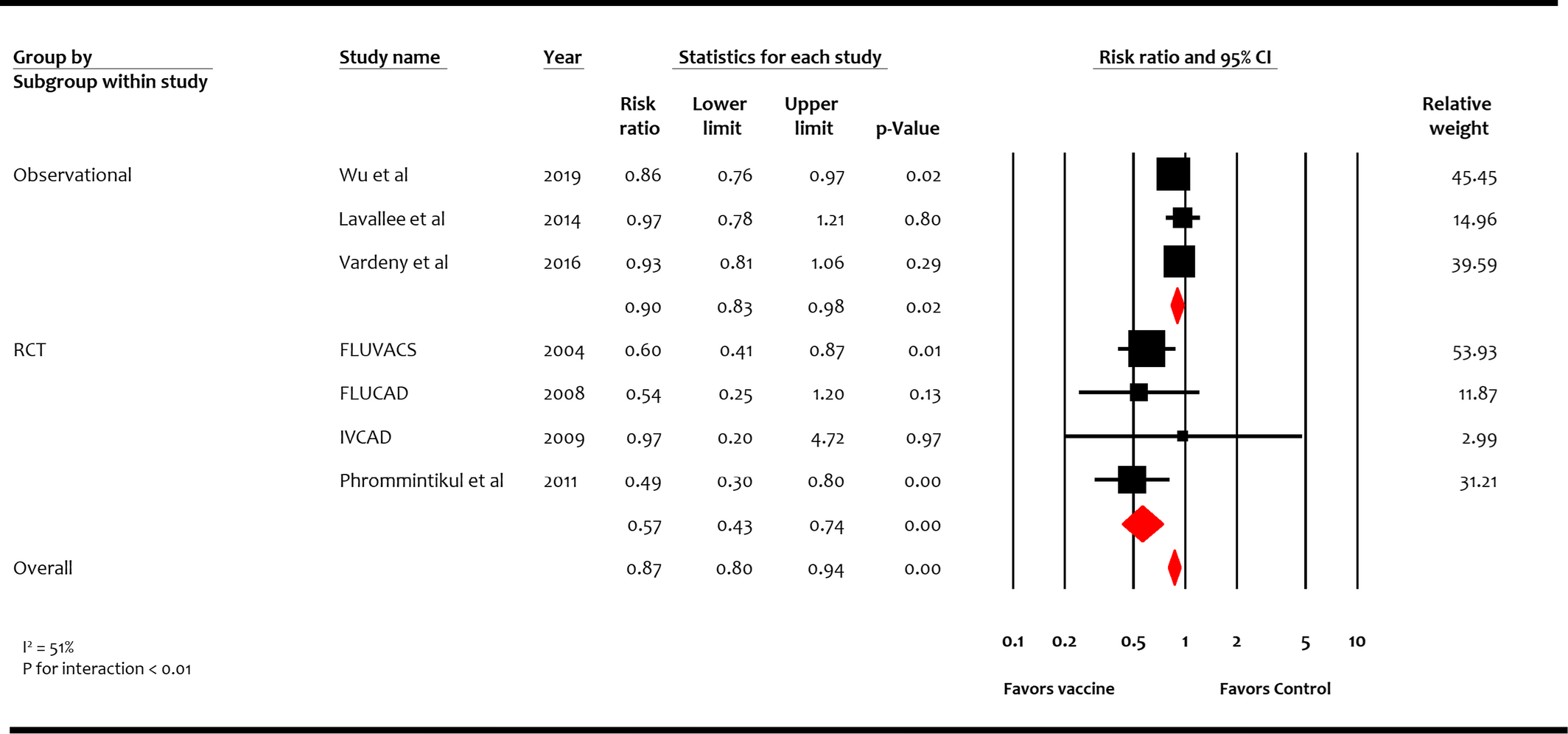
中位随访时间为19.5个月时,与对照组相比,接种流感疫苗与较低的全因死亡率(RR为0.75;95%CI为0.60-0.93 [P=0.01])、心血管疾病死亡率(RR为0.82;95%CI为0.80-0.84 [P<0.001])和主要的不良心血管事件(RR为0.87;95%CI为0.80-0.94 [P<0.001])相关。与对照组相比,接种流感疫苗与心肌梗死降低无统计学相关性(RR为0.73;95%CI为0.49-1.09 [P=0.12])。
由此可见,随机对照试验和观察性研究的数据均支持目前临床威廉亚洲博彩公司 推荐意见,即心血管疾病患者接种流感疫苗以降低死亡率和心血管事件。临床医生和卫生系统应继续推广流感疫苗,作为全面二级预防的一部分。
原始出处:
Siva H. Yedlapati.et al.Effects of Influenza Vaccine on Mortality and Cardiovascular Outcomes in Patients With Cardiovascular Disease: A Systematic Review and Meta‐Analysis.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019636
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#患者死亡#
52
很严谨的学术论文
115
#疾病患者#
64
#AHA#
119
#心血管结局#
88
#血管疾病#
55