Neurology:TSPO PET 有助于诊断 CNS 血管炎
2018-12-21 杨中华 脑血管病及重症文献导读
这个病例提示 TSPO PET 是有助于检测活动性 CNS 炎症,比如怀疑 CNS 血管炎的患者。
67岁,男性。
肺移植后接受免疫抑制剂他克莫司治疗,后来逐渐出现左侧痉挛性偏瘫。
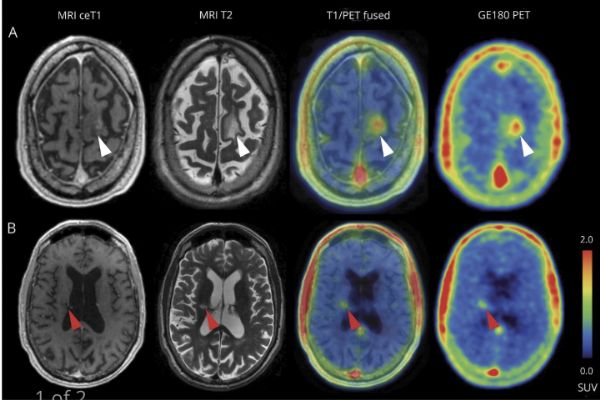
MRI 显示两处弥散抑制,T2高信号伴/不伴部分强化(下图):
[18F]GE-180示踪新型转位蛋白(translocator protein,TSPO)PET 显示双侧 T2高信号病灶区可见示踪剂摄取增加:
TSPO 是活化小神经胶质细胞的过度表达。
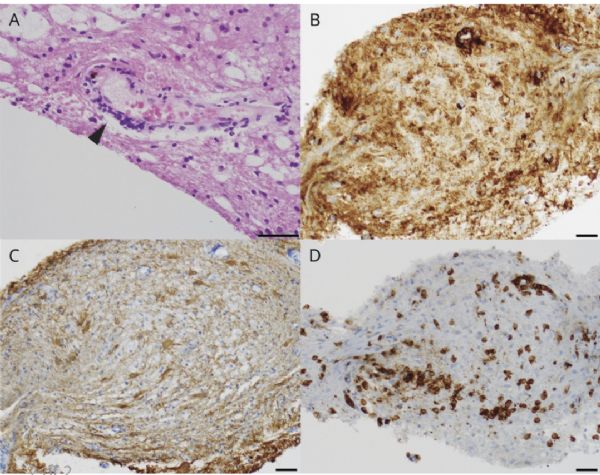
立体定向活检显示他克莫司相关 CNS 血管炎伴小胶质细胞激活。A 图,小血管壁淋巴细胞浸润(箭头,苏木精 & eosin 染色);B 图,小胶质细胞激活(CD3/43染色);C 图,星形胶质细胞活化(胶质纤维酸性蛋白染色);D 图,CD3+ T 细胞浸润。比例尺,100um:
这个病例提示 TSPO PET 是有助于检测活动性 CNS 炎症,比如怀疑 CNS 血管炎的患者。
原始出处:
Christoph Mahler, Marcus Unterrainer, Carolin Muth, et al. Imaging microglial activation in tacrolimus-associated CNS vasculitis with translocator protein PET. Neurology. Nov 2018.
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言






#Neurol#
43
#CNS#
42
#PE#
37
#血管炎#
34
#PET#
49