超声诊断腹膜后平滑肌肉瘤1例
2018-12-28 王豪 中国超声医学杂志
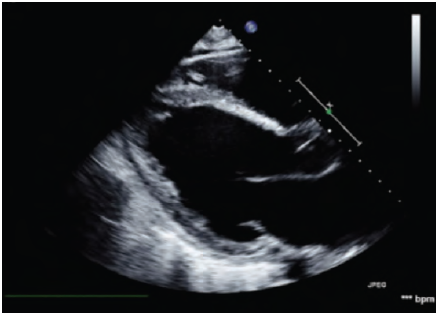
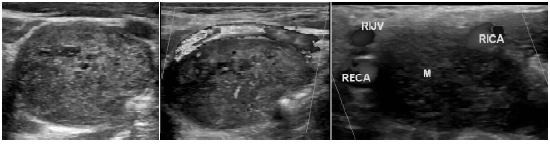
患者男,23岁。发现左侧腰部包块伴腰部隐痛4个余月入院。超声示:左侧输尿管跨髂血管分叉处探及一大小约为59mm×48mm×45mm低回声,形态呈分叶状(图1a)。

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#平滑肌#
55
#腹膜后#
46
#超声诊断#
44
#超声诊断#
30
#腹膜#
38