EUR J Cancer:独立于EGFR的Elk1 / CIP2A信号介导了厄洛替尼衍生物TD52对三阴性乳腺癌细胞的凋亡诱导作用
2017-12-31 MedSci MedSci原创
厄洛替尼可试用于两个或两个以上化疗方案失败的局部晚期或转移的非小细胞肺癌的三线治疗。而厄洛替尼衍生物TD52已经被证明可以用于乳腺癌的治疗。
厄洛替尼可试用于两个或两个以上化疗方案失败的局部晚期或转移的非小细胞肺癌的三线治疗。而厄洛替尼衍生物TD52已经被证明可以用于乳腺癌的治疗。
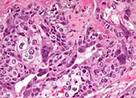
抑癌性蛋白磷酸酶2A(CIP2A)的抑制剂已经作为几种新药用于多种肿瘤的治疗。研究者们在本文中详述了厄洛替尼衍生物TD52的临床效果和作用机制。研究发现TD52处理后的三重阴性乳腺癌(TNBC)细胞中p-EGFR受到显著抑制,且CIP2A显著下调。
研究者们在公共数据库中调研了CIP2A mRNA的表达水平,发现较高水平的CIP2A mRNA与较差的无复发生存期紧密相关。TD52介导的细胞凋亡通常会伴随着CIP2A的下调,因此可以推断CIP2A的过表达保护了TD52介导的细胞凋亡。值得注意的是,蛋白磷酸酶2A(PP2A)的活性在TD52处理的细胞中显著升高。进一步的实验证明,TD52可以通过阻碍转录调节蛋白Elk1与CIP2A启动子的结合进而直接下调CIP2A的转录水平。
综上所诉,独立于EGFR的Elk1 / CIP2A信号通路介导了厄洛替尼衍生物TD52对三阴性乳腺癌细胞的凋亡诱导作用。
原始出处:
Liu, Chun-Yu, et
al. "EGFR-independent Elk1/CIP2A signalling mediates apoptotic effect of
an erlotinib derivative TD52 in triple-negative breast cancer cells."
European Journal of Cancer 2017 72: 112-123. doi.org/10.1016/j.ejca.
本文系williamhill asia 医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#TD52#
63
#衍生物#
0
#阴性乳腺癌#
59
#癌细胞#
58
#厄洛替尼#
64
#三阴性#
51
#GFR#
0