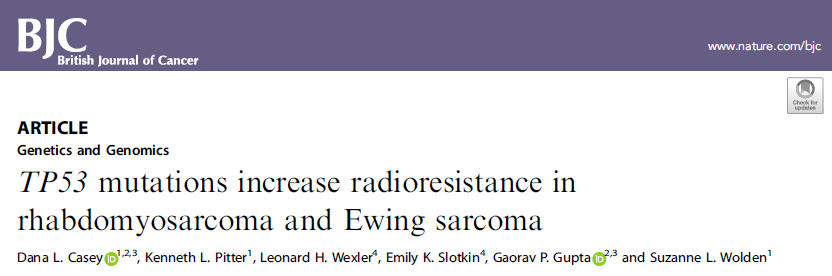
Br J Cancer:TP53突变增加横纹肌肉瘤和尤文肉瘤的放疗抗性
2021-05-30 xiaozeng MedSci原创
目前,包括横纹肌肉瘤 (RMS) 和尤文肉瘤 (ES) 在内的儿科肉瘤复发患者的预后仍然很差,患者的长期存活率很低。
目前,包括横纹肌肉瘤 (RMS) 和尤文肉瘤 (ES) 在内的儿科肉瘤复发患者的预后仍然很差,患者的长期存活率很低。放疗(RT)后失败是疾病复发的常见原因,肿瘤大小和肿瘤位置等临床因素通常与局部肿瘤治疗失败相关。
尽管小儿肉瘤放疗后的反应存在着显著的异质性,但目前在分子水平上尚不清楚是什么驱动了肿瘤组织的放疗敏感性和放疗抗性。考虑到放疗在RMS和ES的主要部位和远端转移部位的治疗中都起着至关重要的作用,因此,进一步了解放疗反应相关的基因组决定因素显得尤为重要。
既往研究显示,p53在DNA修复过程以及对放疗的响应中起着关键作用。在该研究中,研究人员旨在确定进行放疗治疗的RMS和ES患者的TP53突变状态和p53信号通路改变的相关临床表型。
研究人员主要分析了109名接受RMS和ES治疗的患者的286个放射部位。比较了具有TP53突变(n=40)和野生型TP53(n = 246)的肿瘤的放疗控制情况。同时还比较了具有任何p53信号通路改变的肿瘤(n=78)与未发生相关改变的肿瘤(n=208)之间的放疗控制情况。
相关研究示意图
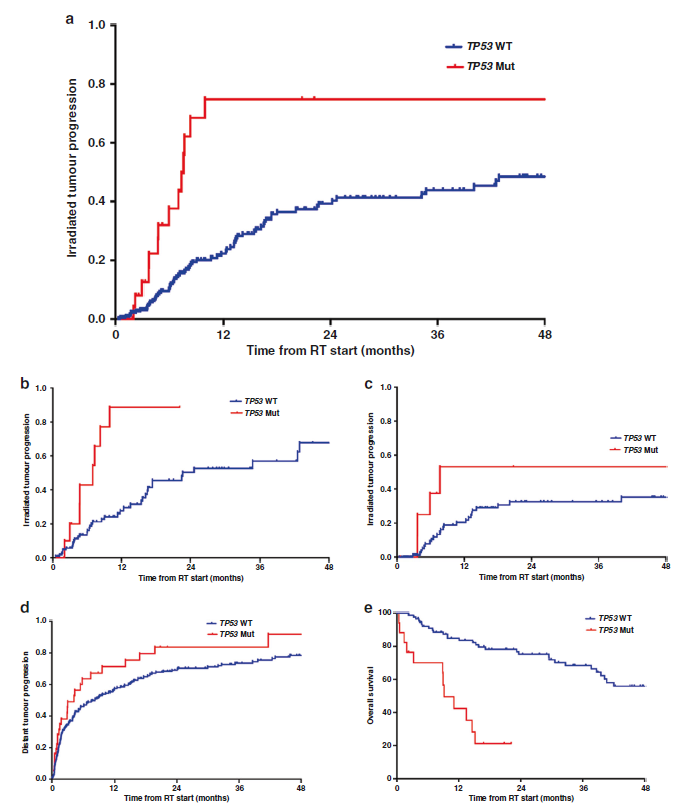
结果显示,患者的中位随访时间为放疗后26个月。研究人员发现,TP53突变与整个队列中较差的放疗肿瘤控制相关(风险比HR=2.8)。具有任何p53信号通路改变的肿瘤也表现出较差的放疗肿瘤控制状况(HR=2.0)。
在多变量分析中,在综合分析了肿瘤组织学、放疗情况、重大疾病的存在和生物学有效剂量之后,TP53突变仍与放疗抗性的表型相关(HR=7.1)。
不同TP53状态患者的放疗肿瘤进展和生存率分析
综上,该研究结果表明,TP53突变与RMS和ES的放疗抗性的增加相关。因此,研究该放疗抗性的新治疗策略对于改善p53突变型RMS和ES患者的临床结局非常重要。
原始出处:
Casey, D.L., Pitter, K.L., Wexler, L.H. et al. TP53 mutations increase radioresistance in rhabdomyosarcoma and Ewing sarcoma. Br J Cancer (20 May 2021).
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#抗性#
62
#p53#
90
#TP53#
127
#尤文肉瘤#
73
赞
98