Sci Signal:p53受癌细胞中的有氧糖酵解作用的调控
2020-06-03 MedSci原创 MedSci原创
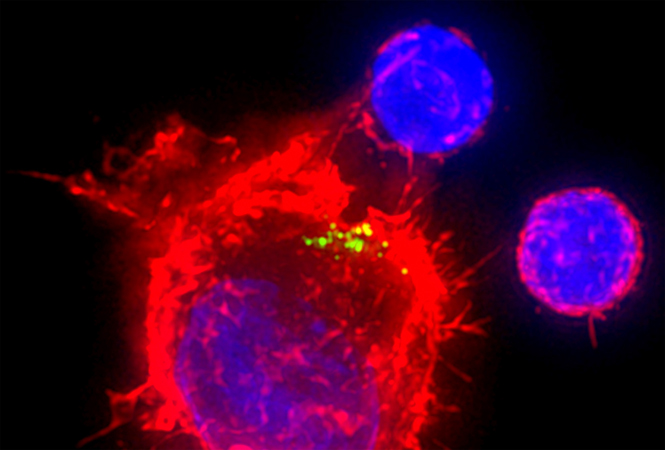
利用人乳腺癌细胞模型,研究人员确定了一种途径,其中线粒体外NADH:NAD+比值的变化通过CtBP家族的NADH敏感转录调控剂控制p53的丰度和活性。
癌细胞中的高糖酵解率是许多人类肿瘤的一个既定特征,它为迅速增殖的癌细胞提供了可用作合成代谢途径的前体的代谢产物。高糖化率的维持依赖于乳酸脱氢酶催化的NAD+的再生,因为NADH:NAD+比例的增加会抑制GAPDH。
最近,利用人乳腺癌细胞模型,研究人员确定了一种途径,其中线粒体外NADH:NAD+比值的变化通过CtBP家族的NADH敏感转录调控剂控制p53的丰度和活性。NADH-free形式的CtBPs与p53结合伙伴HDM2合作,抑制p53功能,而NADH-free形式的CtBPs在高度糖酵解细胞中的缺失导致p53的蓄积。
研究人员表明,这一途径代表了一种 "糖酵解应激反应",通过增加NADH:NAD+比例启动保护性的p53反应,使细胞避免了代谢供需不匹配造成的细胞损伤。
原始出处:
Charles N. Birts et al. p53 is regulated by aerobic glycolysis in cancer cells by the CtBP family of NADH-dependent transcriptional regulators, Science Signaling (2020). DOI: 10.1126/scisignal.aau9529
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













不错
71
#Signal#
60
#Sign#
57
#癌细胞#
56
#糖酵解#
61
#p53#
47