JCH:21年研究!夜间脉压高,心血管死亡风险增加160%,全因死亡风险增加72%
2021-07-07 “心关注”公众号 “心关注”公众号
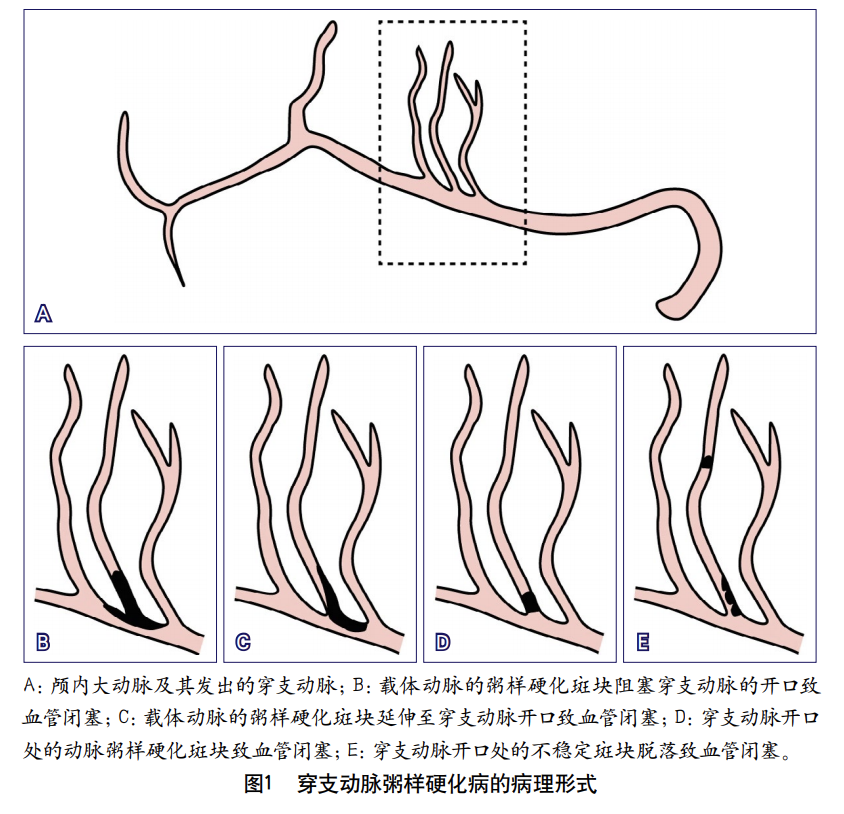
脉压=收缩压-舒张压,可作为衡量动脉粥样硬化程度的指标之一。脉压随年龄的增长而增加,过高的脉压值,更是心血管事件和全因死亡风险的独立危险因素,尤其是在中老年人群中。
脉压=收缩压-舒张压,可作为衡量动脉粥样硬化程度的指标之一。脉压随年龄的增长而增加,过高的脉压值,更是心血管事件和全因死亡风险的独立危险因素,尤其是在中老年人群中。
芬兰卢奥大学学者评估了在中年人群中,将24小时动态脉压值作为长期心血管事件和全因死亡率预测因子的可行性,研究结果已发表在世界高血压联盟官刊《JCH》上。

研究人员选取了1991-1993年间接受连续24小时动态血压监测的900人(女性占比50.4%),依据脉压值由低到高分为T1、T2、T3三组。平均随访时间21.1年,统计各组人群的致命性/非致命性心血管事件、死亡和全因死亡发生情况。
01
死亡 VS 幸存者基线特征
在900例参与者中,共统计到203例死亡。相比幸存者,死亡人群的以下特征更为突出:
① 年龄较大,BMI较高,吸烟比例、饮酒量较高;
② 冠心病、糖尿病、既往卒中或短暂性脑缺血发作的比例更高;
③ 无论日间、夜间、24小时还是诊室测量结果,脉压、收缩压、舒张压均更高;
④ 空腹血糖、胰岛素、甘油三酯更高,HDL-C更低,但总胆固醇、LDL-C无差异。
02
脉压与心血管死亡率
在调整了年龄、性别、患病情况、生活方式等各基线参数后,发现:
在所有参与者中,24小时动态脉压与心血管死亡风险无关。区分性别时,24小时动态脉压与男性心血管死亡风险独立相关,高24小时动态脉压值的男性,心血管死亡风险增加了198%,女性未显着增加。
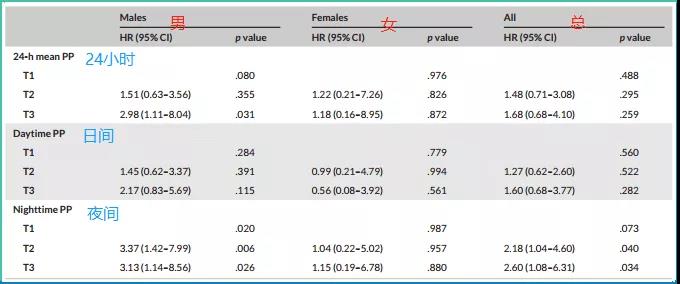
图片:24小时脉压值与21年内心血管死亡风险高低的关联
在所有参与者中,夜间脉压值高的人群,心血管死亡风险显着增加了160%。区分性别时,夜间脉压仅与男性心血管死亡风险独立相关,高夜间脉压值的男性,心血管死亡风险增加了213%。
而日间脉压,无论是所有参与者,还是在男性或女性中,均与心血管死亡风险无显着关联。
03
脉压与心血管事件
同样是使用多变量Cox回归模型,结果却并未发现24小时、日间、夜间脉压与心血管事件发生风险之间存在关联。
当针对男女不同性别人群时,同样未发现二者之间的关联。
04
脉压与全因死亡率
高24小时脉压值的男性,全因死亡风险增加140%;
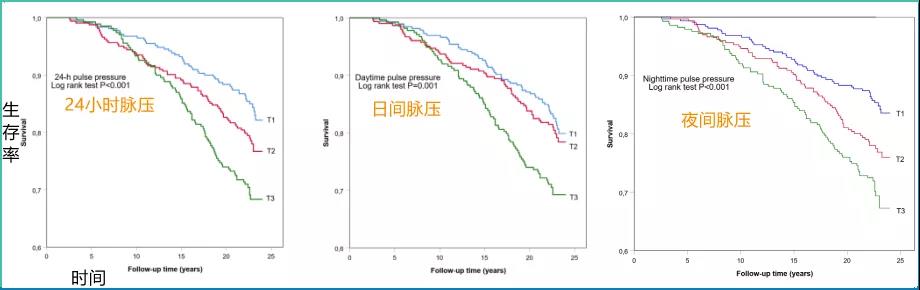
图片:脉压值高低与全因死亡率的KM生存分析(注:T1、T2、T3三组的脉压值范围由低到高,在24小时、日间、夜间中,各组的脉压范围并不相同)
高夜间脉压值的人群,全因死亡风险增加72%,男性增加126%;
日间脉压及其他,与全因死亡风险无显着关联。
该研究认为,在中年人群中,夜间高脉压值,预示着长期心血管死亡和全因死亡风险的增高。
原始出处:
Pivi A. Lempiinen, et al. Nighttime ambulatory pulse pressure predicts cardiovascular and all-cause mortality among middle-aged participants in the 21-year follow-up. JCH. First published: 03 July 2021.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#全因死亡风险#
56
#死亡风险#
53
#心血管死亡#
60
#心血管死亡风险#
65