science advance: 癌细胞操纵神经系统?纳米颗粒来解救! 成功抑制了肿瘤的发展和转移
2021-10-19 MedSci原创 MedSci原创
乳腺癌是女性最常见的癌症之一,尽管在诊断和治疗的突破,但是全球每年仍然约有 685,000 名妇女死于乳腺癌。
乳腺癌是女性最常见的癌症之一,尽管在诊断和治疗的突破,但是全球每年仍然约有 685,000 名妇女死于乳腺癌。
近期发表在Science Advances 上的一项研究发现了一种创新的乳腺癌治疗方法,该疗法基于靶向神经系统的镇痛纳米粒子。研究结果表明,该新技术显著抑制了肿瘤的发展和向肺部、大脑和骨髓的转移。
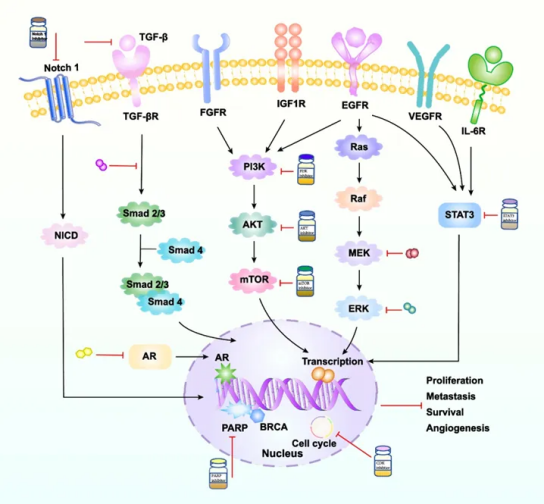
在该研究中,研究人员发现,三阴性乳腺癌细胞(4T1)与它们周围的神经细胞有一种相互的关系:三阴性乳腺癌细胞(4T1)和神经元之间的信号传递涉及刺激神经元生长的细胞因子的分泌。反之,神经元通过分泌神经递质刺激4T1的增殖、迁移和生存。这表明肿瘤微环境中的神经元促进了癌症的发展。因此,其局部靶向治疗具有潜在的临床效益。

基于这些发现,研究人员开发了一种通过神经细胞靶向肿瘤的治疗方法。
他们将药物分子封装在纳米颗粒中。该纳米粒子模拟细胞膜,并涂有特殊的聚合物,可将它们伪装成免疫系统,并能在血液中长时间循环。

在体外,100纳米的纳米颗粒很容易被初级神经元吸收,从神经元体和沿轴突贩运。研究员设计了加载了非阿片类镇痛剂布比卡因的PEG化脂质纳米颗粒,然后将含有麻醉剂的纳米颗粒注射到血液中, 纳米粒子通过血液流向肿瘤,在癌组织中的神经细胞周围积聚,并麻痹局部神经以及神经细胞与癌细胞之间的通讯。
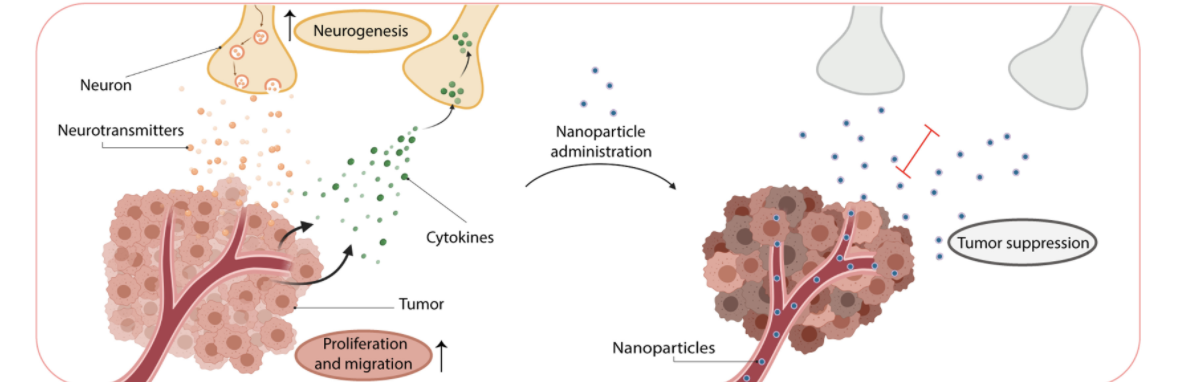
实验结果发发现布比卡因遏制了神经元的生长和与癌细胞的信号传递,抑制了癌细胞的活力。在体内,布比卡因负载的纳米粒子静脉注射抑制了正位三阴性乳腺癌肿瘤的神经元,抑制了肿瘤的生长和转移性传播。
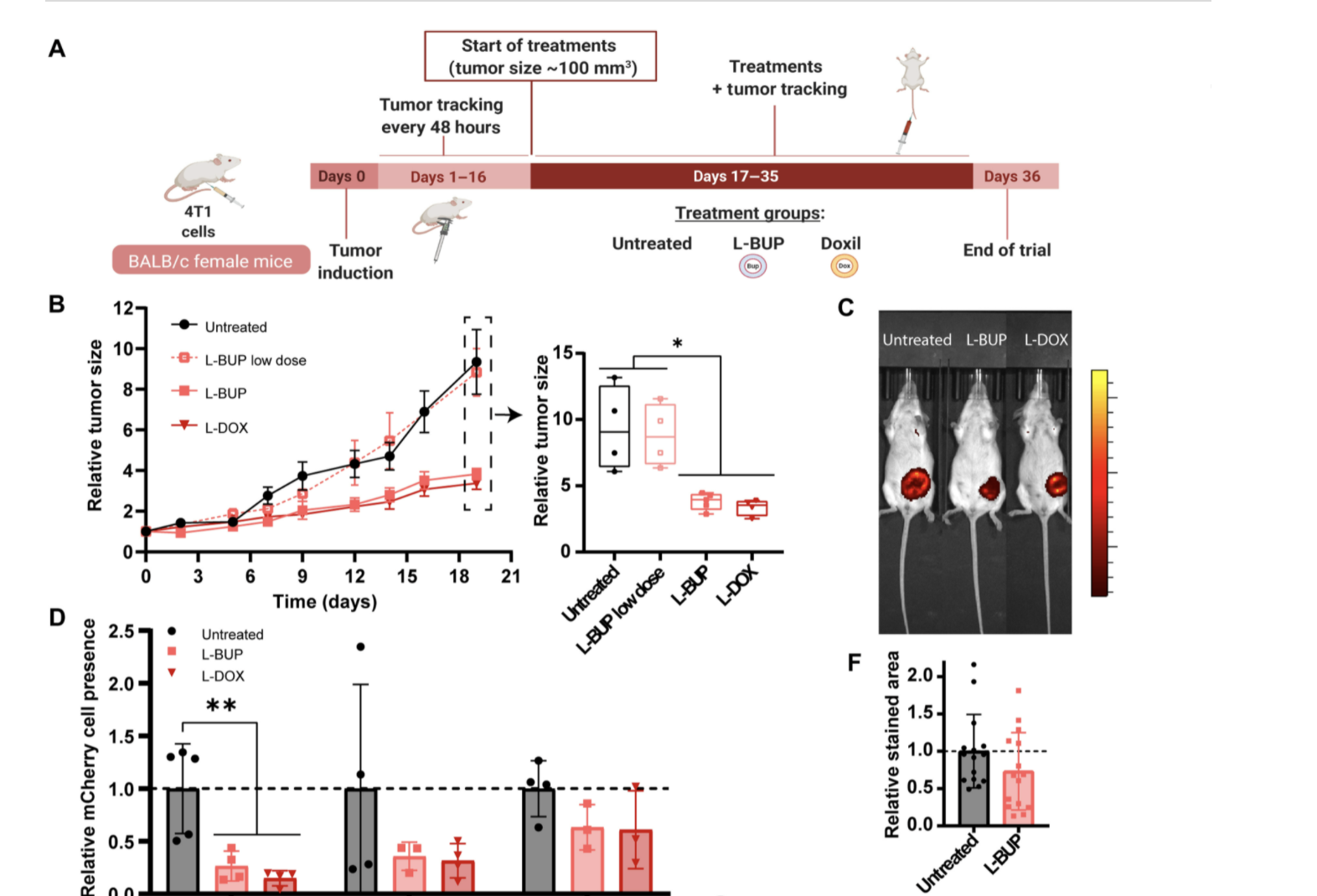
Maya Kaduri 说,该麻醉颗粒在血液中移动,但不会穿透健康组织。只有当它们到达肿瘤受损的血管时,它们才会泄漏出来。然后聚集在癌组织的神经细胞周围,并麻痹局部神经以及神经细胞和癌细胞之间的交流,从而显着抑制肿瘤发展和向肺、脑和骨髓的转移。
这是一种非常集中和精确的治疗方法,使williamhill asia 能够将大量麻醉剂注入体内,因为不必担心它会伤害神经系统的健康和重要区域。”
总的来说,该研究结果表明,减少肿瘤中的神经参与对治疗癌症很重要。
参考文献:Maya Kaduri et al, Targeting neurons in the tumor microenvironment with bupivacaine nanoparticles reduces breast cancer progression and metastases, Science Advances (2021). DOI: 10.1126/sciadv.abj5435. www.science.org/doi/10.1126/sciadv.abj5435
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言

















#癌细胞#
77
#神经系统#
66
#纳米颗粒#
83
#SCIE#
76