卵巢癌新药olaparib获3期临床突破
2017-03-16 健康一线 健康一线
据外媒报道,近日阿斯利康公司宣布一项卵巢癌3期临床试验的重磅消息。Lynparza是一种多聚二磷酸腺苷核糖聚合酶(PARP)抑制剂,它可阻断参与修复受损DNA的酶。这款药物适用于高度预处理的与BRCA基因缺陷相关的卵巢癌。 本次临床试验则再次彰显了LYNPARZA的潜力。在这项名为SOLO-2的3期临床试验中,经独立调查(Blinded Independent Central

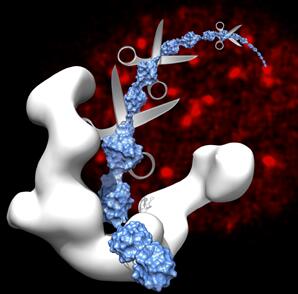
近日阿斯利康公司宣布一项卵巢癌3期临床试验的重磅消息。olaparib(商品名Lynparza)是一种多聚二磷酸腺苷核糖聚合酶(PARP)抑制剂,它可阻断参与修复受损DNA的酶。这款药物适用于高度预处理的与BRCA基因缺陷相关的卵巢癌。
本次临床试验则再次彰显了LYNPARZA的潜力。在这项名为SOLO-2的3期临床试验中,经独立调查(Blinded Independent Central Review)评估,接受LYNPARZA片剂(300毫克,每日两次)治疗的患者,中位数无进展生存期达到了30.2个月。与之相比,服用安慰剂的患者中位数无进展生存期仅为5.5个月。这意味着,患者的中位无进展生存期延长了24.7个月(HR 0.25; 95% CI 0.18-0.35; P<0.0001),两年有余!
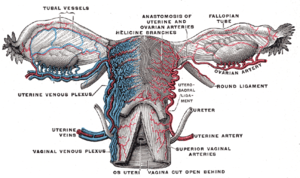
在世界范围内,卵巢癌是女性癌症患者最常见的死因之一。在女性生殖系统癌瘤中占第3位,次于宫颈癌和宫体癌。近几年来,由于对宫颈癌及宫体癌的防治,取得了一定的成效,而有关卵巢癌的防治方面收效相对较小。所以在妇女生殖系统癌瘤中,卵巢癌是造成死亡原因最高的一种肿瘤。在带有BRCA突变等特定遗传性基因异常的情况下,女性发生卵巢癌的风险会显着增加。由阿斯利康研发的LYNPARZA是一款口服聚ADP核糖聚合酶(PARP)抑制剂,可以利用肿瘤DNA损伤反应(DDR)通路缺陷来杀伤癌细胞。
与先前的胶囊相比,LYNPARZA片剂并未出现意料外的副作用--在非血液相关的症状中,患者出现的最常见的副作用是头晕、乏力、呕吐;与血液相关的常见副作用包括贫血、中性粒细胞减少以及血小板减少。这与LYNPARZA胶囊的已知副作用较为一致。
原始出处:
Lheureux S, Lai Z, Dougherty BA, Runswick S, Hodgson D, Timms KM, Lanchbury JS, Kaye SB, Gourley C, Bowtell DD, Kohn EC, Scott CL, Matulonis UA, Panzarella T, Karakasis K, Burnier JV, Gilks B, O'Connor MJ, Robertson JD, Ledermann J, Barrett JC, Ho TW, Oza AM. Long-term responders on olaparib maintenance in high-grade serous ovarian cancer: Clinical and molecular characterization. Clin Cancer Res. 2017 Feb 21. pii: clincanres.2615.2016.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#LAP#
57
#3期临床#
54
#olaparib#
59
#卵巢癌新药#
60
#APA#
39
又一个靶向制剂诞生。
1