JAMA Cardiol:耄耋之年房颤患者服用小剂量依度沙班的疗效和安全性
2022-04-25 Nebula MedSci原创
80岁及以上的房颤患者,服用小剂量依度沙班可降低卒中和全身栓塞事件的发生风险,且不显著增加出血事件风险
房颤 (AF) 的患病率随年龄的增长而增加,AF和年龄都是卒中的独立危险因素。长期口服抗凝药物 (OAC) 对房颤患者预防脑卒中是至关重要的。OAC在高龄房颤患者 (≥80岁) 和出血风险高的患者中的有效性和安全性需要进一步明确。
本研究是对于2016年8月5日-2019年12月27日期间开展的一项随机、双盲、安慰剂为对照的3期临床试验的预定亚组分析,旨在探索极低剂量依度沙班(15 mg)vs 安慰剂在三个年龄段(80-84岁、85-89岁、≥90岁)房颤患者中的效果和安全性。
本次分析纳入了不能服用标准剂量OAC的老年人;不能服用标准剂量OAC的原因包括肌酐清除率降低(<30 mL/min)、低体重(≤45 kg)、内脏出血史、持续使用非甾体类抗炎药或同时应用抗血小板药物。受试者被随机分至依度沙班组(15 mg/天)或安慰剂组。主要疗效终点是卒中或全身性栓塞的复合结局;主要安全终点是大出血。
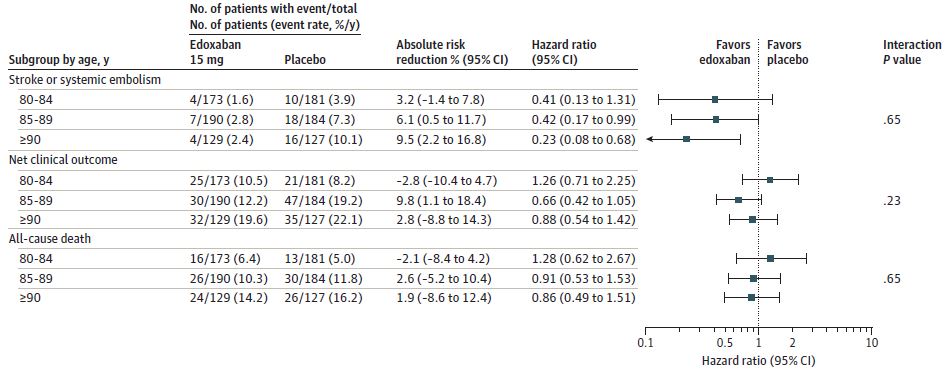
疗效终点
共纳入了984位患者(平均年龄:80-84岁组,82.2岁;85-89岁组,86.8岁;≥90岁组,92.3岁;57.4%的女性)。在安慰剂组,卒中或全身性栓塞的估计发生率随着年龄的增长而增加,80-84岁组,3.9%/人·年;85-89岁组,7.7%/人·年;≥90岁组,10.1%/人·年。15 mg/天的依度沙班降低了所有年龄段患者卒中或全身栓塞的发生率,且与年龄没有相互作用(三个年龄段的风险比依次是0.41[p=0.13]、0.42[p=0.05]和0.23[p=0.008])。
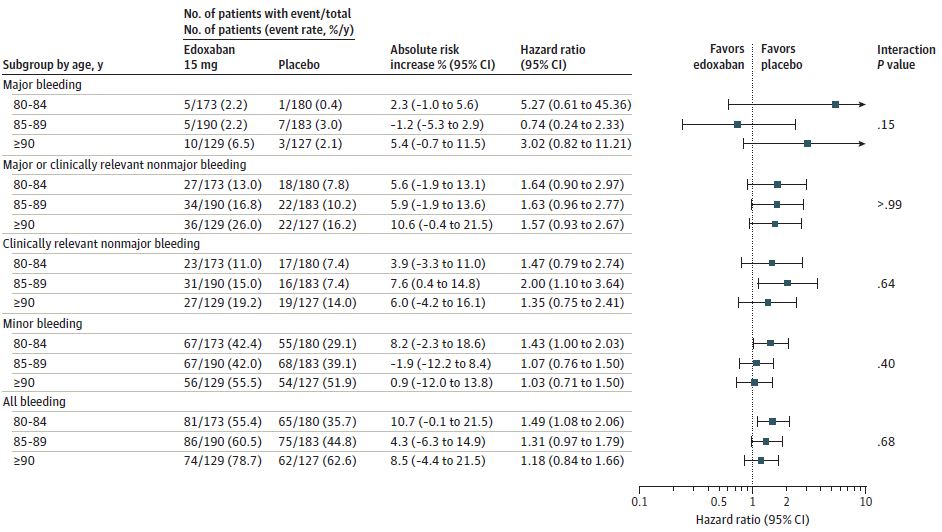
安全性终点
艾多沙班组大出血、严重或临床相关非严重出血事件的发生率较高,但差异无统计学意义,且与年龄没有相互作用。在所有年龄段,依度沙班组和安慰剂组的全因死亡事件发生率没有差异。
综上,该研究结果提示,不能采用标准剂量OAC治疗的80岁及以上的房颤患者,服用小剂量依度沙班(15 mg/天)可降低卒中和全身栓塞事件的发生风险,且不显著增加出血事件风险。
原始出处:
Kuroda Masaru,Tamiya Eiji,Nose Takahisa et al. Effect of 15-mg Edoxaban on Clinical Outcomes in 3 Age Strata in Older Patients With Atrial Fibrillation: A Prespecified Subanalysis of the ELDERCARE-AF Randomized Clinical Trial.[J] .JAMA Cardiol, 2022, https://doi.org/10.1001/jamacardio.2022.0480
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#疗效和安全性#
71
#小剂量#
80
#Cardiol#
61
#依度沙班#
108
#房颤患者#
97
#房颤#可
0
认真学习~
0
学习一下
72
JAMA上文章都是顶级的,谢谢williamhill asia 及时上新
48