JCEM:嗜铬细胞瘤和交感神经节旁瘤的发病率和临床表现
2021-01-23 MedSci原创 MedSci原创
嗜铬细胞瘤和交感神经节旁瘤(PPGL)是分泌儿茶酚胺的罕见肿瘤,但最近的研究表明其发病率正在增加。PPGL的发病率1977年至2015年增加了4.8倍。
嗜铬细胞瘤和交感神经节旁瘤(PPGL)是分泌儿茶酚胺的罕见肿瘤,但最近的研究表明其发病率正在增加。传统上,PPGL患者具有阵发性症状和高血压,但有关PPGL患者临床表现的现有数据均来自转诊中心。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究为一项基于人群的研究,旨在归纳PPGL患者的临床表现和发病率的时间趋势。
研究人员对1977-2015年期间在丹麦确诊的567例PPGL患者进行回顾性队列研究,并从192名患者组成的亚组的医疗记录中收集了临床数据。研究人员计算了全国人群的年龄标准化发病率(SIR)和患病率,并根据临床数据对亚组的表现进行了描述性统计。
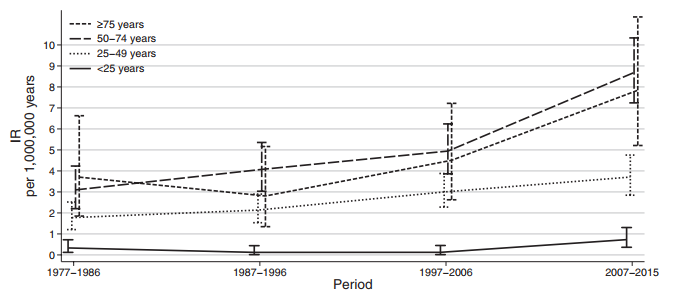
该疾病的SIR从1977年的每百万人每年1.4人(95%CI为0.2-2.5)增加到每百万人每年6.6人( 2015年,95%CI为4.4-8.7),相当于增长了4.8倍。该增加主要是由于偶然发现小于4 cm的肿瘤,并且在50岁以上没有儿茶酚胺过量的阵发性症状或局限性发作的患者被诊断所致。

2015年12月31日,PPGL的患病率为每百万居民64.4人(95%CI为57.7-71.2)。在192例临床数据中,有171例(89.1%)患有单侧嗜铬细胞瘤,而单侧副神经节瘤(n=13,6.8%)和多灶性PPGL(n=8,4.2%)很少见。
由此可见,PPGL的发病率1977年至2015年增加了4.8倍。
原始出处:
Tali Cukierman-Yaffe.et al.The Relationship between Glucose Control & Cognitive Function in People with Diabetes after a Lacunar Stroke.JCEM.2021.https://doi.org/10.1210/clinem/dgaa965
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#发病率#
50
#JCEM#
56
#JCE#
43
学习了
97
#细胞瘤#
47
文献引用错了
102