Plos One:CRE定植一定会发展成CRE感染吗?
2017-12-09 检索:乔甫 翻译:张渝婧 审稿:孔懿 SIFIC感染官微
许多文章都曾探讨定植CRE的患者对其进一步发展为CRE感染的可能性,但多数文章是在发生CRE感染暴发后进行的回顾性调查,并且所涉及的科室种类繁多。
本文通过观察性研究ICU的危重患者在定植CRE或Ceph-R(第三/第四代头孢菌素耐药的肠杆菌科细菌)后,30天内对其发展成相应感染的影响,以及90天内对其死亡率的影响。作者进行了庞大数据的回顾,以及系统性的分析,得出了非常有趣的结果。希望读者们能从中有所收获。
背景
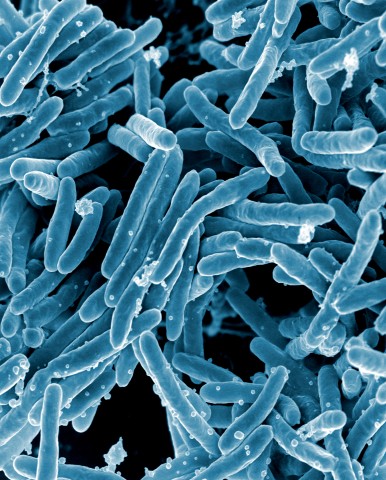
目前,碳青霉烯类抗生素耐药的肠杆菌(CRE)已成为公共卫生安全的巨大威胁。肠道定植CRE已被认为是全身感染CRE的一个重要危险因素,但是未将其与第三/第四代头孢菌素耐药的肠杆菌科细菌(cephalosporin-resistant,Ceph-R)定植进行比较。同时,williamhill asia
仍不清楚由定植引起患者不良结局的风险,尤其是入住ICU的危重病人。
方法
本次队列研究的对象为2013年4月—7月间ICU病房内的直肠CRE或Ceph-R定植病人。收集患者的临床特征变量,并评估CRE或Ceph-R定植与30天内CRE全身感染(初始结局)以及90天内死亡率(第二结局变量)之间的关系。
结果
ICU住院的338名患者中,94位(28%)存在CRE或Ceph-R定植。随后30天内,采集试子发现有26人发生CRE感染,其中有47%(N=17/36)为之前CRE定植病人,3%(N=2/58)为Ceph-R定植。在90天的随访期内,CRE定植、Ceph-R定植、无任何定植的患者中分别有36%(N=17/36)、31%(N=18/58)和15%(N=37/244)死亡。
多因素分析发现,CRE定植是30天中CRE感染的独立危险因素(aOR 10.8, 95%CI 2.8±41.9, p=0.0006),而Ceph-R定植则不是(aOR 0.5, 95%CI 0.1±3.3, p=0.5)。单因素分析发现CRE定植增加了患者90天死亡率(p=0.001),而在多因素分析中既往住院史和入住内科ICU史是90天内死亡的独立危险因素,而CRE定植只是接近具有统计学意义(aOR 2.3, 95%CI 1.0±5.3, p=0.056)。
结论
本研究显示ICU患者中定植CRE增加了患者感染CRE和死亡的风险。未来的研究中,williamhill asia
将进一步探讨针对CRE定植患者如何经验性选择抗生素,以及建立去定植的有效方法。
讨论
直肠定植CRE已经被认为是造成患者随后感染CRE的重要流行病学危险因素。在最近的一篇荟萃分析中,患者定植造成累积感染率达到16.5%。然而,这些涵盖各种临床科室的文章,主要是在感染暴发时的进行研究,几乎没有只关注ICU患者的研究,限制了普遍性。在williamhill asia
研究的ICU患者中,williamhill asia
发现CRE定植是30天内(通过直肠拭子采集发现感染)获得感染的重要影响因素。研究中,近50%的CRE定植患者在30天内发展为CRE感染,这意味着与非定植患者相比,其感染几率增加了10.8倍。
值得一提的是,在所有由CRE定植发展为CRE感染的患者中,除了一位患者其他人的定植菌与感染菌同种同源。这可能进一步暗示医务人员习惯在定植患者身上经验性使用抗生素。考虑到最常见的感染是肺炎,误吸胃肠道内容物很可能是这群危重患者肠道定植菌发展为感染的潜在机制。曾经接受内镜或结肠镜检查同样是造成CRE感染的影响因素。有趣的是,有报道称由于ERCP造成的产Ceph-R细菌和CRE的感染暴发(最终归因于难以对内镜进行灭菌处理),但在williamhill asia
的研究中ERCP或EUS都不是定植的影响因素。
更有趣的是,Ceph-R定植与后续30天内的CRE感染并不显著相关,虽然拥有几乎相同的流行病学危险因素。定植Ceph-R和定植CRE的ICU患者拥有相互重叠的危险因素,这些因素也预示着那些造成CRE定植的危险因素并不足以造成CRE感染,先前的定植才是更重要的。williamhill asia
注意到在Ceph-R定植和CRE感染之间存在一个反向关系,它们在多因素分析中无显著差异。这可能意味着Ceph-R细菌与CRE共享一个肠道内定植位点,一旦Ceph-R先定植,则反而在一定程度上保护机体免受CRE的定植和感染。但最终是宿主和病菌的什么因素导致定植转变为感染尚不清楚。
有关CRE定植后的不利结局没有被完全报道。一项报告合并分析了三篇文章的数据,发现定植或感染患者的死亡率为10%,但是由定植发展为感染的患者死亡率更高(30-75%)。在第二阶段的分析中,williamhill asia
研究了90天内死亡的危险因素。在多因素比较中,只有入住内科ICU,CCIS评分,和曾经住院这三个因素最有可能影响90内的死亡率。有趣的是,那些在单因素分析中显示Ceph-R或CRE定植与死亡密切相关的因素在多因素分析中却未见,特别是考虑到导致ICU患者死亡的潜在因素众多。
原始出处:
McConville TH, et al. Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS ONE. Oct 2017
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言






#Plos one#
53
一起学习一下
0
学习了
76
#CRE#
64
值得关注的问题
97
了解了解.继续关注
75
谢谢分享.学习了
103