Front Oncol:安罗替尼联合PD-1抑制剂治疗晚期实体肿瘤有效且毒性可控
2021-10-10 yd2015 MedSci原创
该研究表明,安罗替尼联合PD-1抑制剂治疗晚期实体肿瘤具有一定疗效并且毒性可控。
免疫检查点抑制剂(ICIs)与抗血管治疗联合是目前肿瘤治疗的方向。安罗替尼(Anlotinib (AL3818))是一种新型的多靶点酪氨酸激酶抑制剂(TKI),靶向血管内皮生长因子受体(VEGFR),抑制肿瘤生长。通过抑制血管内皮生长因子来调节免疫微环境,可增强免疫检查点抑制剂的活性。近期,Frontiers in Oncology杂志上发表了安罗替尼联合免疫治疗在晚期实体肿瘤患者的安全性和疗效。
自2019年1月以来,26例晚期肿瘤患者接受了治疗,包括肺癌、胆囊癌、子宫内膜癌、胃癌、胰腺癌、阴茎癌和黑色素瘤。患者接受联合安罗替尼(12mg),每天1次,第1天至第14天(21天为一个疗程),每3周加抗PD-1抗体,直到进展或无法忍受的毒性。在治疗的第一年,每6周进行一次影像学检查。前瞻性地采集患者血液样本。流式细胞术检测基线及治疗后血清白细胞介素(IL)-2、IL-4、IL-6、IL-10、肿瘤坏死因子-a (TNF-a)、干扰素-g (IFN-g)及循环免疫细胞亚群。
纳入26例患者中,13名男性(50.0%)和13名女性(50.0%),中位年龄为66岁(37-77岁)。值得注意的是,53.8%的患者年龄在65岁或以上,25例(96.2%)患者的ECOG评分为0-1,1例(3.8%)患者的ECOG评分为2。腺癌有14例(53.8%),鳞癌有4例(15.4%),肉瘤有3例(11.5%)。接受安罗替尼一线治疗有5例(19.2%),二线治疗13例(50.0%),三线及以上治疗8例(30.8%)。9例患者接受12mg的安罗替尼治疗,14例接受10mg的安罗替尼治疗,3例接受8mg的安罗替尼作为起始剂量。PD-1抑制剂中,接受sintilimab、camrelizumab、toripalimab、nivolumab或pembrolizumab治疗的患者人数分别为15(57.7%)、5(19.2%)、3(11.5%)、2(7.7%)和1(3.8%)例。
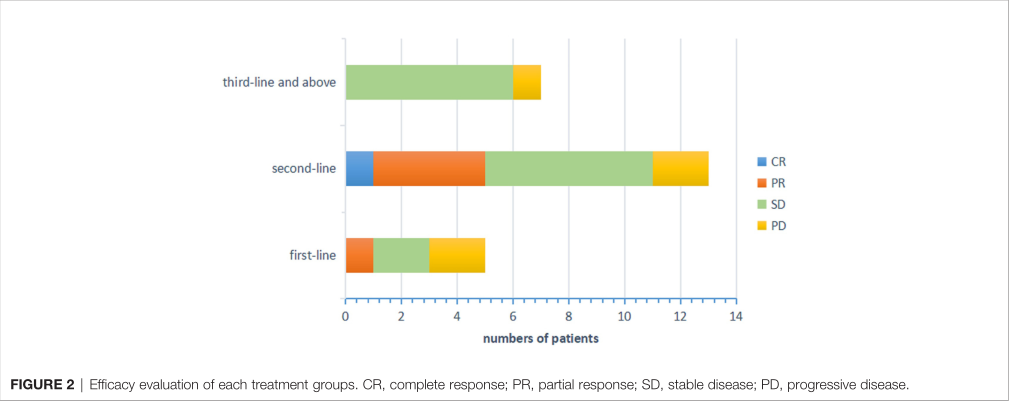
该研究主要终点是ORR和DCR。26例患者的ORR为23.08% (CR为3.85%,PR为19.23%)。DCR为80.77% (3.85% CR, 19.23% PR, 57.69% SD)。一线、二线、三线及以上联合方案治疗的患者分别为19.23%、50.00%和30.77%。DCR分别为60.00%(3/5)、84.62%(11/13)和87.50%(7/8)。亚组分析显示,接受不同治疗线患者的DCR差异无统计学意义(p=0.354)。肝转移患者的ORR为37.5% (3/8),DCR为87.5%(7/8)。
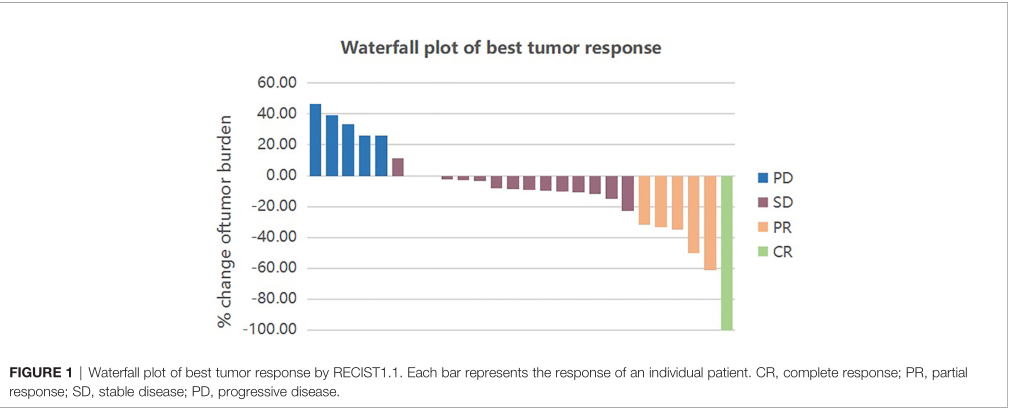
中位随访时间为9.0个月(范围为4.97- 20.43个月),8例患者死亡。所有患者的中位无进展生存期(PFS)为4.77个月(95% CI: 4.10-5.44个月)。达到CR患者为7.33个月,PR组为5.23个月(95% CI: 0.94 ~ 11.80个月),SD组为4.95个月(95% CI: 4.61 ~ 5.29个月),PD组为1.67个月(95% CI: 0.91 ~ 2.40个月)。PFS差异有统计学意义(P=0.013)。为了确定哪些患者能从安罗替尼联合抗PD-1抗体中获得更大的临床获益,将获得CR或PR或SD的患者定义为有反应组,PD患者定义为无反应组。反应组患者的PFS明显更长,为5.00个月(95% CI: 4.31-5.69个月),而无反应组为1.67个月(95% CI: 0.94-2.40个月)。PFS差异有统计学意义(P=0.001)。与ECOG相关的PFS也有显著差异(P=0.001)。而中位OS尚未达到。

总的来说,46.15%的患者经历了治疗相关的AEs。9例1-2级不良事件(34.62%)和3例3级不良事件(11.54%),但未观察到4级或5级事件。最常见的不良反应是疲劳(19.23%)、食欲下降(15.38%)和手足综合征(15.38%)。最严重的不良事件是3级手足综合征和高血压(11.54%)。
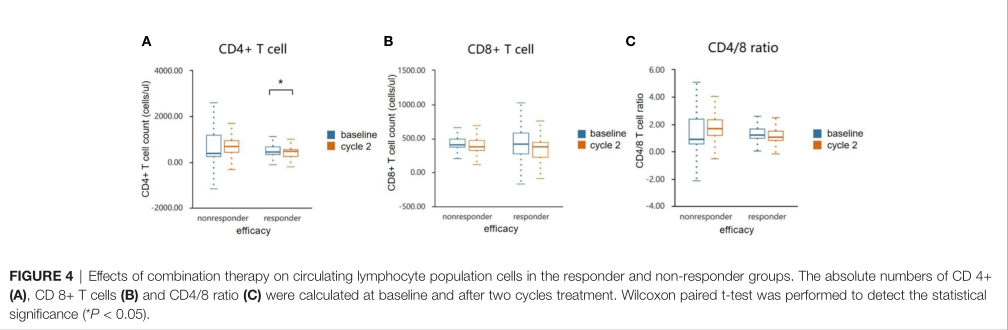
与无反应组相比,安罗替尼联合抗PD-1抗体使血液中CD4+ T细胞明显下降(p<0.05),两组CD8+ T细胞均下降。反应组CD4+/CD8+ T细胞比值降低,而非应答组CD4+/CD8+ T细胞比值则相反。但是,两组间CD8+ T细胞变化量及CD4/8比值无显著性差异。
综上,该研究表明,安罗替尼联合PD-1抑制剂治疗晚期实体肿瘤具有一定疗效并且毒性可控。
原始出处:
Yuan M, Zhu Z, Mao W, Wang H, Qian H, Wu J, Guo X and Xu Q (2021) Anlotinib Combined With Anti-PD-1 Antibodies Therapy in Patients With Advanced RefractorySolid Tumors: A Single-Center, Observational, Prospective Study. Front. Oncol. 11:683502. doi: 10.3389/fonc.2021.683502
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#抑制剂#
126
#晚期实体肿瘤#
56
#Oncol#
66
#PD-1抑制剂#
64
#实体肿瘤#
74
卡通了吧我舅舅他们他拒绝
71
学习学习
79