高危患者LDL-C≥1.4 mmol/L,推荐联合用药降脂!ACC发布非他汀药物应用路径共识
2022-08-28 中国循环杂志 中国循环杂志
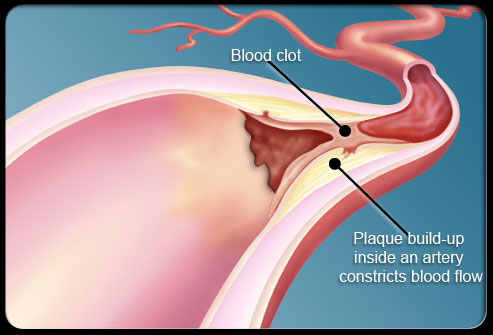
共识建议,对于接受高剂量他汀类药物治疗的临床极高危ASCVD患者、ASCVD患者、临床诊断或基因检测确诊家族性高胆固醇血症患者,若LDL-C≥1.4 mmol/L推荐联用非他汀类药物治疗。
点击下方链接查看共识原文
2022 ACC专家共识决策路径:降低低密度脂蛋白胆固醇的非他汀类治疗在动脉粥样硬化性心血管疾病风险管理中的作用(2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: A Report of the American College of Cardiology Solution Set Oversig)
8月25日,美国心脏病学会(ACC)发布了应用非他汀类药物降低LDL-C管理动脉粥样硬化性心血管疾病(ASCVD)风险的专家共识决策路径文件。
共识建议,对于接受高剂量他汀类药物治疗的临床极高危ASCVD患者、ASCVD患者、临床诊断或基因检测确诊家族性高胆固醇血症患者,若LDL-C≥1.4 mmol/L(或非HDL-C ≥ 2.2 mmol/L),推荐联用非他汀类药物治疗。
1、坚持改善生活方式,并坚持给予威廉亚洲博彩公司 推荐的他汀类药物治疗;
风险增强因素包括:
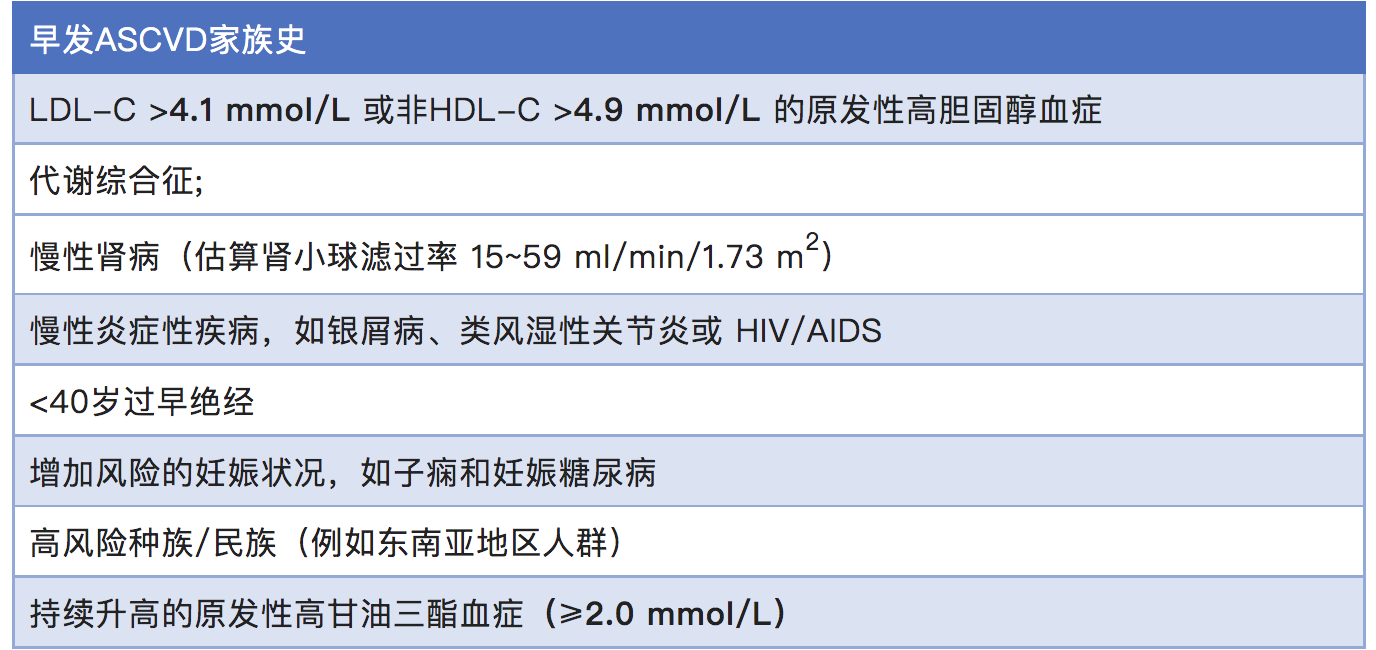
高敏 C 反应蛋白≥2 mg/dL,脂蛋白(a)≥50 mg/dL或≥125 nmol/L,载脂蛋白 B >130 mg/dL,踝臂指数<0.9,也提示ASCVD风险增加;
要注意控制其他心血管病风险因素;
在考虑增加非他汀类药物的应用时,医患决策要考虑所用药物的潜在获益与危害,以及患者偏好、治疗费用;
要对生活方式改变、药物应用依从性及治疗效果进行监测;
对于杂合子家族性高胆固醇血症(HeFH)和纯合子家族性高胆固醇血症(HoFH) 患者必要时给予血浆净化疗法;
洛美他派(lomitapide)、依维苏单抗(evinacumab)均仅限于HoFH;
对PCSK9单克隆抗体依从性较差,或者产生不良反应,或无法自行注射的患者,可考虑使用inclisiran进行治疗;
对于在使用最大剂量他汀类药物和(或)联合用依折麦布及贝培多酸情况下,加用PCSK9单克隆抗体或inclisiran。
目前尚无证据或机制上的合理性可证明,联用PCSK9单克隆抗体与inclisiran可获得LDL-C降低的额外获益或更好心血管结局转归,因此,若要使用inclisiran,应替换PCSK9单克隆抗体,而非联用。
2. 临床极高危ASCVD患者,或者基线LDL-C>4.9 mmol/L的ASCVD患者,或者家族性高胆固醇血症患者,若接受最大耐受剂量他汀类药物治疗,并已联用PCSK9单克隆抗体或依折麦布,仍未充分降低LDL-C,考虑启动非他汀药物治疗。
一些患者可能仅非增加一种药物能够达到需要更大程度降低LDL-C,为尽快降低心血管事件复发风险,可考虑同时增加两种药物。
其中的选择可包括高强度或最大耐受剂量他汀类药物联用依折麦布,或最大耐受剂量他汀类药物联合或联合依折麦布,再联用PCSK9单克隆抗体。
如果患者LDL-C降低<50%或LDL-C仍>1.4 mmol/L,可以考虑添加贝培多酸。
如果对于PCSK9单克隆抗体依从性较差、或存在不良反应,或无法自行注射,可考虑使用inclisiran进行治疗。
3. 对于有或无临床ASCVD的患者,以及临床或基因诊断确诊HoFH患者,如果应用最大耐受剂量他汀类药物治疗联合或不联合依折麦布、PCSK9单克隆抗体和(或)贝培多酸情况下,仍不能充分降低LDL-C,可考虑在血脂专家指导下给予依维苏单抗(evinacumab)、洛美他派(lomitapide)或 LDL血浆净化疗法。
4. 基线 LDL-C>4.9 mmol/L的非极高危ASCVD或临床ASCVD患者,如临床或基因检测未确诊为家族性高胆固醇血症,当 LDL-C>1.8 mmol/L,在应用最大耐受剂量他汀类药物情况下,推荐考虑增加非他汀类药物治疗。
5. 非极高危ASCVD患者,鉴于ASCVD转归的改善,以及在急性冠脉综合征患者中依折麦布联用辛伐他汀较之单用辛伐他汀更胜一筹,可考虑依折麦布每天10 mg作为初始非他汀类药物治疗手段。
6. 40~75岁糖尿病患者是至少中等强度他汀类进行一级预防的候选人群。
对于10年ASCVD风险>7.5%或伴有糖尿病特异性风险增强因素的患者应考虑使用高强度他汀类药物。
如果糖尿病患者10年ASCVD风险>20%,且在应用最大耐受剂量他汀类药物治疗情况下,LDL-C降低<50%和(或)LDL-C>1.4 mmol/L(或非HDL-C>2.6 mmol/L),可考虑加用依折麦布。
7. 对于无糖尿病患者的一级预防,中高强度他汀类药物的应用是基础。
如果10年ASCVD风险>20%,且在应用最大耐受剂量他汀类药物治疗情况下,LDL-C仍未能充分降低 ,可考虑加用依折麦布。
8. 对于冠状动脉钙化评分为1~99 AU或<75th百分位数,及冠状动脉钙化评分为100~999 AU或>75th百分位数的患者,均建议使用中高强度他汀类药物治疗。
如果未能实现 LDL-C降低>50%或LDL-C>1.8 mmol/L,则可以考虑加用依折麦布。
如果冠状动脉钙化评分>1000 AU,并且患者在最大耐受剂量他汀类药物联合依折麦布治疗中未能实现LDL-C降低>50%或LDL-C>1.8 mmol/L,则可以考虑添加PCSK9单克隆抗体。
9. 临床ASCVD患者、基线 LDL-C>4.9 mmol/L、家族性高胆固醇血症患者、高危糖尿病患者、高危一级预防患者或有明显亚临床动脉粥样硬化证据患者,如无法耐受循证证据为基础的可耐受他汀类药物治疗,可考虑使用非他汀类药物治疗,以进一步降低LDL-C。
治疗药物的选择取决于患者基线水平ASCVD风险以及支持所用药物的证据基础。
对于患有持续性或严重高甘油三酯血症者,可参阅2021年ACC发布的关于高甘油三酯血症管理的专家共识决策路径文件
原始出处:
Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2022;Aug 24
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#高危患者#
75
#ACC#
93
#LDL#
57
#联合用药#
73
赞
66