转子间骨折髓内钉主钉置于股骨颈轴线中心力学强度更佳
2012-08-20 水天之间 丁香园
髓内钉是手术固定股骨转子间不稳定骨折的常见内置物。在髓内钉手术操作中,将拉力主钉放置于最佳位置非常重要。以往应用滑动钢板(SHS)治疗股骨转子间骨折时,控制好尖顶距(TAD,tip-apex distance)是防止固定失败的重要因素。但对于髓内钉固定,拉力主钉的最佳位置尚存有争议,有人认为拉力螺钉应该沿股骨头轴线置入,并尽量深的放置,也有人认为拉力螺钉应该放
髓内钉是手术固定股骨转子间不稳定骨折的常见内置物。在髓内钉手术操作中,将拉力主钉放置于最佳位置非常重要。以往应用滑动钢板(SHS)治疗股骨转子间骨折时,控制好尖顶距(TAD,tip-apex distance)是防止固定失败的重要因素。但对于髓内钉固定,拉力主钉的最佳位置尚存有争议,有人认为拉力螺钉应该沿股骨头轴线置入,并尽量深的放置,也有人认为拉力螺钉应该放置于股骨头截面的下方部分。
最近,加拿大多伦多大学医院骨科Paul等对此问题进行了一项生物力学研究。该研究目的在于评价拉力螺钉在股骨头中不同位置(上、下、前、后)所产生的最大机械强度(mechanical stiffness)和失效载荷(load-to-failure)。另外研究还评估了髓内钉机械强度及失效载荷与5项独立放射学测量指标之间的相关性。
该实验应用30例合成股骨建立股骨不稳定转子间骨折模型,采用Gamma3髓内钉固定,头钉位置分别为:上方、下方、前侧、后侧、中心。在X线正侧位片上测量尖顶距和参考距-尖顶距(calcar referenced tip-apex distance,CalTAD)。对标本轴向、侧向弯曲及扭转载荷进行测试,然后在轴向位置上测量失效负载。应用方差分析和线性回归分析进行数据的统计学处理。
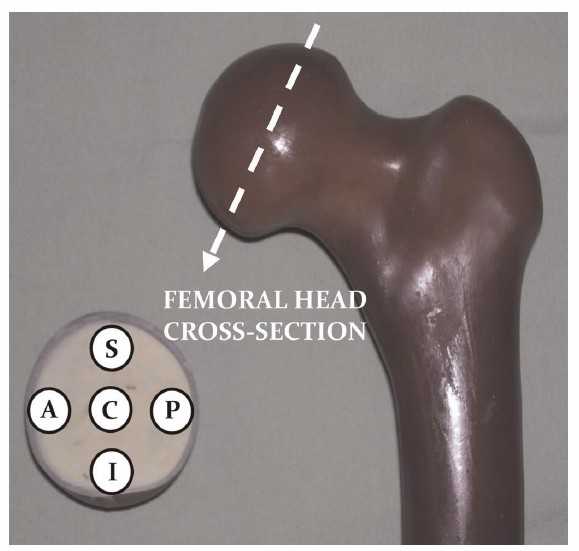
图1:合成股骨模型及横断面图片显示拉力螺钉在股骨头中五种不同位置: S,上方;I,下方;A,前方;P,后方;C,中心。
图2:股骨粗隆间骨折模型正位像,骨折线A:粗隆间骨折线,骨折线B:股骨距内侧缘骨折线。
图3:直线相关分析所侧二两的五种放射学指标:(A)前后位平片计算的尖顶距(TADAP),(B)前后位平片计算的参照距-(CalTADAP),(C)侧位片计算的尖顶距(TADLat),(D)尖顶距(TAD)公式,(E)CalTAD的计算方法。Dtrue为拉力螺钉的直径(如,10.5mm)。

图4:轴向、侧方、扭转力学测试的位置。应用相同的方案监测完整的股骨和髓内钉结构。
图5:拉力螺钉位于上方(S)、下方(I)、前方(A)、后方(P)、中心(C)五个位置的平均强度: 轴向(蓝色柱)、侧方弯曲(红色柱)、扭转(绿色柱)。
表1:生物力学指标(因变量)与放射学指标(自变量)的直线相关分析

图6:轴向强度分别与(A)正位片参照距-尖顶距(CalTADAP)、和(B)参照距-TAD(CalTAD)的关系。
图7:拉力螺钉在股骨头不同位置的失效载荷强度:上方(superior), 下方(inferior ),前方(anterior),后方(posterior), 中心(central) 。数值为均数±1个标准差。
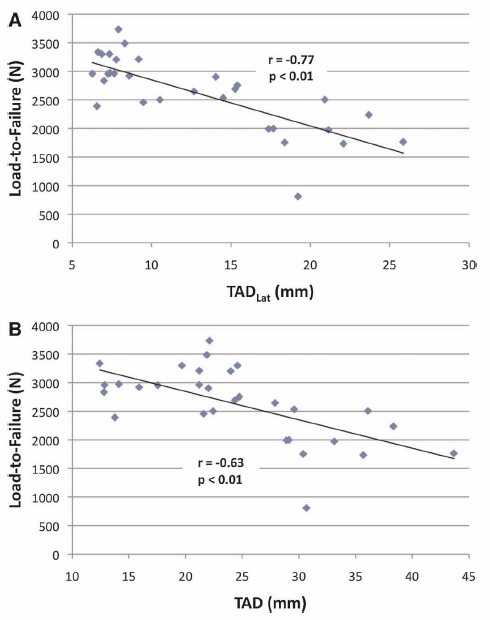
图8:失效载荷分别与(A)侧位片尖顶距(TADlat)和(B)尖顶距(TAD)的关系。
实验结果显示,在轴向强度方面,拉力螺钉位于下方时显着强于上方(P < 0.01)、前侧(P = 0.02)及后侧(P = 0.04)。在扭转强度方面,拉力螺钉位于上方位置时显着小于其他位置(四组对比中P < 0.01)。侧方弯曲强度方面,各位置无显着差异。在失效载荷方面,拉力螺钉位于上方和中心位置显着强于前侧(P < 0.01 and P = 0.02)和后侧位置(P < 0.01 and P = 0.05)。呈显着负相关的是:固定强度与头钉在正侧位片上的CalTAD;失效载荷与在侧位片上头钉到股骨颈中心的距离。
编译者按:本文所测量的参考距-尖顶距(calcar referenced tip-apex distance,CalTAD),结合了原有TAD的概念与九宫格分区头钉位于下方的概念,极有可能成为未来尖顶距研究的发展方向。
原文链接:
Kuzyk PR, Zdero R, Shah S, Olsen M, Waddell JP, Schemitsch EH. Femoral head lag screw position for cephalomedullary nails: a biomechanical analysis. J Orthop Trauma. 2012 Jul;26(7):414-21.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#转子间#
54
#股骨颈#
58
#髓内钉#
54
#股骨#
38