Pediatr Allergy Immunol:lgE敏感和鼻炎对炎症生物标记和肺功能的影响
2018-11-08 AlexYang MedSci原创
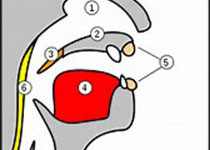
过敏性和非过敏性鼻炎与更差的哮喘控制相关。然而,lgE敏感和/或鼻炎是怎样与肺功能相关的还不清楚。最近,有研究人员评估了鼻炎和敏感对肺功能的影响,包括了患有或不患有哮喘患者的气道系统周边和炎症生物标记情况。研究人员将哮喘、鼻炎和敏感组合的小组与健康的对照进行了比较。研究发现,在只患有哮喘(调整后平均差-2.8%-单位(95% CI -4.7;-1.0), p<0.01))、哮喘和敏感(-2.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#DIA#
44
#PE#
51
#ALL#
49
#生物标记#
55
#lgE#
49
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
86