Nature:揭示离子通道TRPM2是身体检测环境温度所必需的
2016-08-20 佚名 生物谷
随着气温在整个英国攀升,williamhill asia 检测和躲避过于温暖的地方的能力在调节williamhill asia 的体温中起着至关重要的作用。然而,在此之前,很少有人了解williamhill asia 皮肤中的感觉神经元负责检测炎热气温的分子机制。 在一项新的研究中,来自英国伦敦国王学院的研究人员揭示出一种被称作TRPM2的基因启动小鼠体内的“炎热”信号,从而促使它们寻找更加凉爽的环境。当移除这个基因时,这些小鼠就不能够区分凉爽温度和炎热温度。相关研究结果于2016年
随着气温在整个英国攀升,williamhill asia
检测和躲避过于温暖的地方的能力在调节williamhill asia
的体温中起着至关重要的作用。然而,在此之前,很少有人了解williamhill asia
皮肤中的感觉神经元负责检测炎热气温的分子机制。
在一项新的研究中,来自英国伦敦国王学院的研究人员揭示出一种被称作TRPM2的基因启动小鼠体内的“炎热”信号,从而促使它们寻找更加凉爽的环境。当移除这个基因时,这些小鼠就不能够区分凉爽温度和炎热温度。相关研究结果于2016年8月17日在线发表在Nature期刊上,论文标题为“The TRPM2 ion channel is required for sensitivity to warmth”。
已知一些“瞬时感受器电位(Transient Receptor Potential, TRP)”蛋白被高温引发的痛觉水平所激活。这些蛋白能够传导正电荷离子穿过细胞膜,因而能够改变神经细胞的内部电压。这种电压上的变化接着触发神经活性,因此,产生高温(如触摸滚烫的水壶)引发的痛觉。然而,之前的研究并未揭示可能被更加温和的不触发痛觉的温度所激活的离子通道。
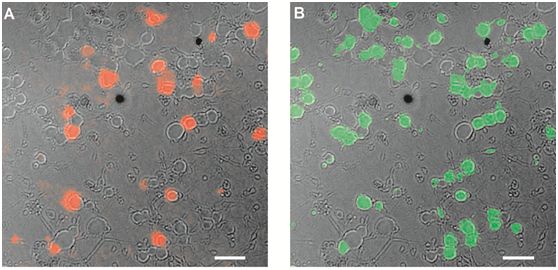
在这项新的研究中,来自伦敦国王学院的Chun-Hsiang Tan博士和Peter McNaughton教授鉴定出一种被称作TRPM2的离子通道,其中在此之前,TRPM2并未发现与温度检测存在关联。在分离到这种新的感知温度的离子通道后,他们移除一组小鼠体内的TRPM2基因,然后当它们在33°C or 38°C的表面上行走时,将它们的行为与正常的小鼠进行比较。他们发现正常的小鼠偏好33°C较为凉爽的温度,躲避38°C较为炎热的温度,然而TRPM2基因被剔除的小鼠不能够区分这两种温度。
Tan博士说,“移除这些小鼠体内的TRPM2基因会破坏它们检测不触发痛觉的温度的能力,但是它们利用其它已知的受体检测引发痛觉的高温的能力并没有受到影响。这揭示出williamhill asia 如何能够在感觉层面上检测太热的环境。”
McNaughton教授说,“williamhill asia 证实TRPM2基因在有意识到地检测温度中发挥着重要作用,而且也在无意识地调节体温中发挥着作用。在未来的研究中,探究TRPM2基因是否也通过调节出汗和皮肤中的血管收缩在控制williamhill asia 的体温中发挥着无意识到的作用将是非常有趣的。”
原始出处
Chun-Hsiang Tan & Peter A. McNaughton.The TRPM2 ion channel is required for sensitivity to warmth.Nature.2016
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#Nat#
35
#TRPM2#
52
这篇威廉亚洲官网 写的真好,带给williamhill asia 新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
59
这篇威廉亚洲官网 写的真好,带给williamhill asia 新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
49
#体检#
42
#离子通道#
49
这个实验没有做过!
33
阅读了,谢谢!
42
学习起来
53