Front Cell Dev:银屑病患者外周血不变性自然杀伤T细胞调节异常
2022-02-28 医路坦克 MedSci原创
银屑病是一种常见的免疫介导的皮肤病,涉及T细胞介导的免疫,本文探讨了银屑病患者外周血NKT细胞的表达及Suckinumab对其的影响。

银屑病是一种常见的免疫介导的皮肤病,涉及T细胞介导的免疫。不变自然杀伤T细胞(INKT)是一种独特的淋巴细胞亚群,具有NK细胞和T细胞的共同特性和表达表面标志。已有报道表明,NKT细胞调控多种炎症性疾病的发生发展。IL-17是银屑病发病机制中的一个关键细胞因子,也是一个重要的治疗靶点。Suckinumab是一种针对IL-17A的全人IgG1型κ抗体,从而拮抗IL-17的生物学效应。
目的:探讨银屑病患者外周血NKT细胞的表达及Suckinumab对其的影响。
williamhill asia 检测了40例中重度斑块型银屑病患者和40例性别、年龄匹配的健康对照者外周血单个核细胞(PBMC)中NKT细胞、Tregs、幼稚和记忆性CD4+和CD8+T细胞的频率及其细胞因子的产生。williamhill asia 进一步采集了另外15名中到重度斑块型银屑病患者的外周血,这些患者接受Suckinumab治疗,并在基线和第12周评估iNKT细胞在PBMCs中的比例。
结果:银屑病患者外周血单个核细胞中CD4+T细胞、CD8+T细胞和Tregs细胞的频率与正常人相当,而Th17细胞、Tc1细胞和Tc17细胞的频率在银屑病患者中升高。银屑病患者外周血NKT细胞和CD69+iNKT细胞频率明显降低。银屑病患者NKT2细胞和NKT17细胞均增高,但NKT2细胞vsiNKT17细胞比例明显降低。经Suckinumab治疗后,患者外周血单个核细胞中NKT细胞比例增加,NKT17细胞比例下降。
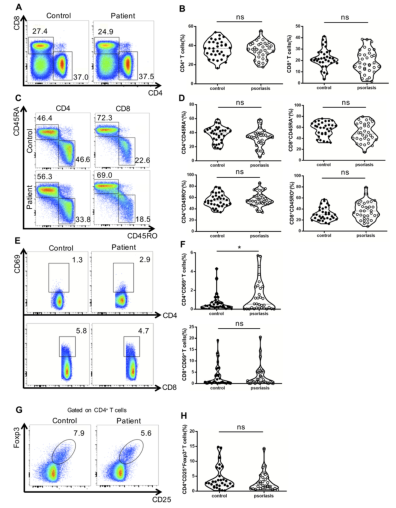
图1 外周血中常规T细胞和Treg细胞的分布。(A)流式细胞术分析中重度斑块型牛皮癣患者和健康对照组外周血单个核细胞中CD4+和CD8+T细胞的分布。(B)显示中重度斑块型牛皮癣患者与健康对照组CD4+和CD8+T细胞频率的个体结果。(C)流式细胞术分析记忆(CD45RO+)和幼稚(CD45RA+)CD4+。(E)流式细胞术分析中重度斑块型银屑病患者和健康对照组外周血单个核细胞中CD69+和CD8+T细胞的表达。(F)显示中重度斑块型银屑病患者与健康对照组CD69+CD4+T细胞和CD69+CD8+T细胞频率的个体结果。(G)CD4+CD25+Foxp3+的流式细胞术分析。数据显示平均值+SEM.p-值由配对学生t检验确定。NS,无显著性,*p<0.001,**p<0.01,*p<0.0001。
根据银屑病患者经Suckinumab治疗后Th17、Tc17水平升高,NKT细胞活化比例和水平降低,NKT17细胞数量增加,iNKT细胞比例升高,推测调节失调的diNKT细胞可能参与了银屑病的发病机制。Suckinumab可能对NKT细胞起调节作用。
文献来源:Hu Y, Chen Y, Chen Z, Dysregulated Peripheral Invariant Natural Killer T Cells in Plaque Psoriasis Patients.Front Cell Dev Biol 2021;9

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#CEL#
49
#Cell#
50
#Dev#
74
#变性#
64
#外周血#
78