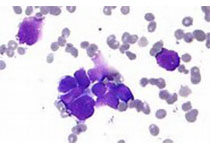
NEJM:Venetoclax治疗急性髓性白血病(AML),III期临床取得正面结果
2020-08-14 Allan MedSci原创
相比于安慰剂联合阿扎胞苷,venetoclax联合阿扎胞苷可延长总体生存期(OS)。
AbbVie今日宣布,《新英格兰医学杂志》(NEJM)刊登了III期临床试验(VIALE-A研究)的结果,该研究评估了venetoclax联合阿扎胞苷治疗初治AML患者的有效性和安全性,结果表明,相比于安慰剂联合阿扎胞苷,venetoclax联合阿扎胞苷可延长总体生存期(OS)。
在多中心VIALE-A研究中,OS是美国研究的唯一主要研究终点,而复合完全缓解率(CR+CRi)是中国、日本、欧盟研究的主要终点。CR+CRi是一个综合评分,反映了完全缓解(CR)和血液系统恢复不完全(CRi)的CR。结果表明,相比于安慰剂联合阿扎胞苷,Venetoclax联合阿扎胞苷可以将死亡风险降低34%(HR=0.66,95%CI:0.52-0.85,p <0.001)。
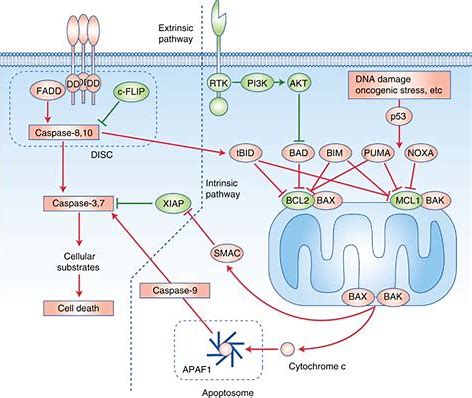
Venetoclax联合治疗组患者的中位OS为14.7个月(95%CI:11.9-18.7),而安慰剂组患者的中位OS为9.6个月(95%CI:7.4-12.7)。此外,接受Venetoclax联合阿扎胞苷治疗的患者中有66.4%(95%CI:60.6-71.9)达到了CR+CRi,而接受安慰剂联合阿扎胞苷治疗的患者中只有28.3%(95%CI:21.1-36.3)达到了CR+CRi(p <0.001)。
VIALE-A试验中观察到的安全性与venetoclax与阿扎胞苷的已知安全性一致。接受venetoclax联合阿扎胞苷治疗的患者中最常见的不良事件(AEs)主要是血液学和胃肠道疾病:血小板减少症(46%)、恶心(44%)、便秘(43%)、中性粒细胞减少症(42%)、发热性中性粒细胞减少症(42%)和腹泻(41%)。在Venetoclax组中有3例患者报告了肿瘤溶解综合征(TLS),而在安慰剂组中则没有。所有这些都是短暂的生化变化,可通过使用尿酸排泄剂解决。
原始出处:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#I期临床#
75
#III#
44
#NET#
43
好
126
#venetoclax治疗#
65
#髓性#
58
#II期临床#
45
#III期#
48
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
104