ASCO GI 2015 :结直肠癌NCCN、NICE、ESMO三大威廉亚洲博彩公司 争鸣
2015-01-20 哈尔滨医科大学附属第二医院肿瘤中心 王贵玉 中国医学论坛报
哈尔滨医科大学附属第二医院肿瘤中心结直肠肿瘤外科 王贵玉 发自美国旧金山 2015年ASCO 结直肠癌内容集中在1月17日一整天,本次会议的一个重要亮点就是结直肠癌美国国立综合癌症网络(NCCN)、英国国家卫生与临床优化研究所(NICE)和欧洲肿瘤内科学会(ESMO)威廉亚洲博彩公司 的制定者共聚一堂,各抒己见。 从左至右:David J. Kerr(NICE威廉亚洲博彩公司 报告者)、Leonard Saltz
哈尔滨医科大学附属第二医院肿瘤中心结直肠肿瘤外科 王贵玉 发自美国旧金山
2015年ASCO 结直肠癌内容集中在1月17日一整天,本次会议的一个重要亮点就是结直肠癌美国国立综合癌症网络(NCCN)、英国国家卫生与临床优化研究所(NICE)和欧洲肿瘤内科学会(ESMO)威廉亚洲博彩公司 的制定者共聚一堂,各抒己见。
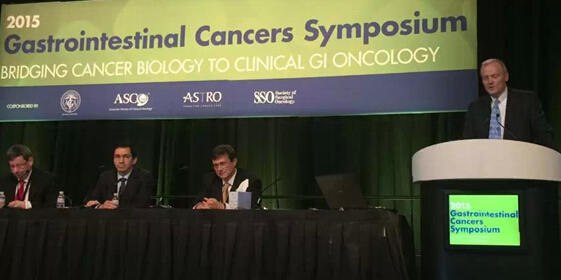
从左至右:David J. Kerr(NICE威廉亚洲博彩公司 报告者)、Leonard Saltz(NCCN威廉亚洲博彩公司 报告者)、Andres Cervantes-Ruiperez(ESMO威廉亚洲博彩公司 报告者)、John Marshall(主持人)
| NCCN威廉亚洲博彩公司 | ESMO威廉亚洲博彩公司 | NICE威廉亚洲博彩公司 |
| NCCN是由21家世界顶级癌症中心组成的非营利性学术联盟,其制订的《NCCN肿瘤学临床实践威廉亚洲博彩公司 》不仅是美国肿瘤领域临床决策的标准,也已成为全球肿瘤临床实践中应用最为广泛的威廉亚洲博彩公司 ,在中国也得到了很多肿瘤医生的认可与青睐,其特点是内容详细,更新周期较短。 |
ESMO 结直肠癌诊疗威廉亚洲博彩公司 由欧洲肿瘤内科学会(ESMO)颁布,其特点是简明扼要,方便指导临床实践,更新周期较长,一般是1年左右。 |
NICE发布的成人结直肠癌诊断和管理临床实践威廉亚洲博彩公司 的特点是对疾病的各阶段提出建议,内容详尽,非常重视花费效率,更新周期非常长,一般3~5年更新一次,在我国认识相对较少。 |
关于遗传性结直肠癌
大约20%的结肠癌伴有家族聚集性,新诊断的腺瘤或者浸润性癌患者,其一级亲属患结直肠癌的风险增加。总之,欧美在遗传性结直肠癌的诊治意见中已基本达到一致,只是个别细节上稍有差异。
对于林奇(Lynch)综合征,NCCN威廉亚洲博彩公司 要求患者在进行基因测序前通常进行两轮筛选:首先是基于家族史,其次是对肿瘤组织进行初始检测。为了甄别那些可能属于Lynch综合征的结直肠癌个体,可以对结直肠癌标本进行两项初始检测:免疫组化检测MMR蛋白表达,因为突变致该蛋白表达缺失;分析微卫星不稳定性(MSI),MSI是MMR 缺失的结果,由于DNA重复单元的插入或缺失而导致,可通过检测肿瘤组织中短的DNA 重复序列的数量改变来判定。如免疫组化结果显示MLH1基因缺失应检测BRAF基因。存在BRAF突变表明MLH1表达下降是由体细胞MLH1基因启动子区域甲基化引起,而并非是通过胚系突变所致。NCCN专家组推荐,应强烈建议在所有50 岁以下的结肠癌患者中开展MMR蛋白检测,原因在于该群体患Lynch 综合征的可能性增加。
在ESMO威廉亚洲博彩公司 中,倾向以70岁作为界限,选择以一种替代策略(即仅对小于70岁的肠癌患者或虽然大于70岁但符合Bethesda标准的肠癌患者进行MMR缺陷检测)代替原有的对所有结直肠癌患者进行MMR缺陷检测。如果该肿瘤检测确实存在MMR缺陷,但未能检测到BRAF突变或是MLH1启动子甲基化,则需行做胚系遗传检测以明确胚系突变。
NICE威廉亚洲博彩公司 关于遗传性结直肠癌并未单独列出。
关于直肠癌术前放化疗
3个威廉亚洲博彩公司 都对局部进展期结直肠癌推荐新辅助放化疗,只是方法和方案上的差别。
NCCN威廉亚洲博彩公司 建议,对于较高局部复发风险的直肠癌,Ⅱ期(T3-4、淋巴结阴性、肿瘤穿透肠壁肌层)或Ⅲ期直肠癌(淋巴结阳性,无远处转移),建议进行新辅助/辅助治疗,通常包括局部区域治疗。传统推荐的放疗剂量是盆腔照射45~50 Gy/25~28f,3或4个照射野,鼓励采用改变体位或其他技术来最大程度减少小肠的照射。5周半的放化疗全部结束后等待5~10周的间歇期再行手术治疗,以便患者能从术前放化疗毒性中恢复。
在NICE威廉亚洲博彩公司 中,根据局部复发的风险定义了3种不同的直肠癌患者高危人群。通过磁共振成像评估局部复发风险,风险度不同的人群其术前的治疗方案不一样,但均须通过多学科协作(MDT)讨论患者的局部复发、短期和长期复风险和远期效果。对于中等风险的可切除直肠癌,可考虑给予短期术前放疗然后立即手术治疗;对于那些介于中、高危复发风险的患者可考虑给予术前放化疗,待肿瘤缩小后再行手术治疗。对于高风险的可切除直肠癌患者,应给予术前放化疗,待肿瘤缩小后再行外科手术治疗。
ESMO威廉亚洲博彩公司 对于高风险的可切除直肠癌患者[cT3(b)cN+]推荐术前放疗,即可采用推荐短程放疗小于1周的短程放疗,总剂量25 Gy、每次5 Gy或长程同步放化疗,总剂量 45~50.4 Gy,每次1.8~2 Gy,联合或不联合5氟尿嘧啶(5-FU)。
关于腹腔镜手术
随着腹腔镜技术在在结直肠癌中的发展和应用,以损伤小、恢复快的优势也日益引起人们的重视。总之,欧美医生在腹腔镜应用到结肠癌上较为推荐,但是在直肠癌的手术中较亚洲医生保守。
只有NICE威廉亚洲博彩公司 明确推荐,将腹腔镜或腹腔镜辅助手术作为结直肠癌可选的手术方案。
NCCN威廉亚洲博彩公司 相对谨慎,指出由经验丰富的外科医生实施的腹腔镜辅助结肠癌手术已被纳入结肠癌手术方式,但腹腔镜直肠癌手术虽然较之前有一定放宽,却仅限于临床研究,仍需要更高级别的证据来支持。
ESMO的专家对于腹腔镜技术特别推荐于结肠癌特别是左半结肠癌,可以安全地开展腹腔镜下结肠切除术。而对于右半结肠癌来说,他们则认为腹腔镜手术的优势不太明显,因为吻合口必须用手缝合,而这需要开腹手术。腹腔镜下结肠切除术的长期结果与传统开腹手术的结果相似。只有符合以下标准,才能实施腹腔镜手术:①技术熟练的外科医生;②没有过去的大手术引起的腹腔黏连;③没有局部晚期疾病,急性肠梗阻或穿孔。
转移性结直肠癌治疗药物的选择
基于目前临床治疗的实践,3个威廉亚洲博彩公司 均推荐基于联合化疗的方案+靶向药物方案,包括氟尿嘧啶类(5‐FU/亚叶酸或卡培他滨)的各种联合化疗及采用奥沙利铂或伊立替康的方案±单克隆抗体。采用西妥昔单抗或帕尼单抗抑制表皮生长因子受体(EGFR)的治疗只适用于野生型KRAS肿瘤,而无论KRAS突变状态如 何,均可使用抗血管内皮生长因子(VEGF)的贝伐珠单抗。 一线化疗后失败的患者,若有较好的体力状态,可考虑改用二线化疗或三线化疗,也同样适用上述原则。
但是3个威廉亚洲博彩公司 也有些微细差别。基于 CALGB80405的研究结果,2015年NCCN结肠癌威廉亚洲博彩公司 重新将含铂类药物的双药方案+西妥昔单抗作为治疗KRAS野生型的转移性结肠癌一线方案。这一点和ESMO威廉亚洲博彩公司 又重新走到了一起。而2014年NICE威廉亚洲博彩公司 仍将西妥昔单抗作为唯一推荐用于一线治疗转移性结直肠癌的靶向药物, 推荐其联合FOLFOX或者FOLFIRI一线治疗晚期结直肠癌。其他如贝伐珠单抗、帕尼单抗作为二线治疗靶向药物。另外,ESMO威廉亚洲博彩公司 推荐瑞戈非尼作为三线或四线支持治疗。(如下图)
关于随访
3个威廉亚洲博彩公司 对于术后随访观察的管理无明显差异,每3~6个月随访一次,肝脏、肺脏CT检查,正电子发射体层摄影(PET)-CT不作为常规随访检查,术后1年内一定复查肠镜。
总之,无论是NCCN、NICE威廉亚洲博彩公司
,还是ESMO威廉亚洲博彩公司
的普及,结直肠癌规范化治疗的理念已被越来越多的临床医师所接受。各国的威廉亚洲博彩公司
是根据本国及本地区的实 际情况制定,大体相同,但仍存在差异,可能与各国国情、人种以及诊治方法等有关。 而做为我国临床医师,更应根据我国的实际情况,选择性地接受各方面的意见,制定出符合我国结直肠癌诊治实际需求的威廉亚洲博彩公司
,使williamhill asia
的结直肠癌诊治更加规范化、 科学化。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#ASC#
44
#SMO#
45
#ESMO#
47
#NICE#
49
#NCCN#
50
#结直肠#
45