Int J Cardiol:疑似急性冠状动脉综合征患者血钾水平与住院期间心律失常和死亡风险
2018-09-30 xing.T MedSci原创
由此可见,入院时高钾血症与疑似ACS患者的院内死亡有关,而低钾血症与心脏骤停和新发房颤有关。
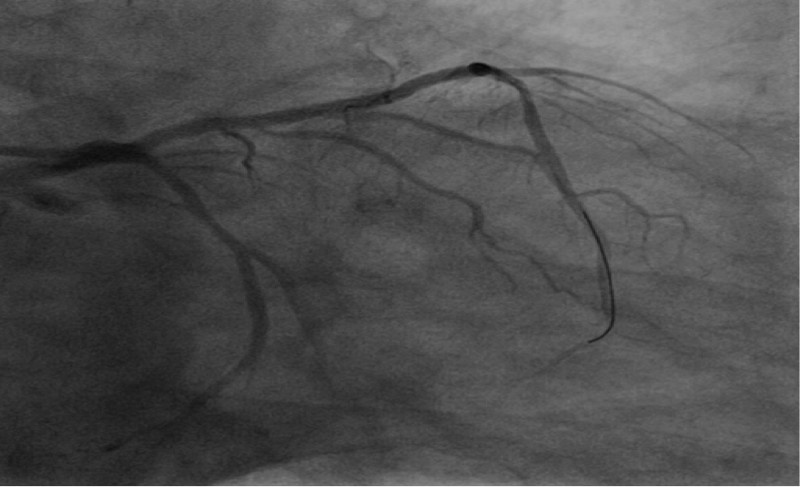
在急性冠状动脉综合征(ACS)患者中,入院时钾失衡与院内心律失常、心脏骤停和死亡有关。然而,尚未考虑ACS的几个重要表现特征和亚型。近日,心血管领域权威杂志International Journal of Cardiology上针对这些问题发表了一篇研究文章。
研究人员招募了2006年至2011年间连续就诊的疑似ACS住院患者(n=32955),并采用logistic回归模型评估了入院时血浆钾水平(参考3.5-4.0mmol/L)与住院结局(包括死亡、心脏骤停、新发房颤以及二度或三度房室传导阻滞)之间的关联。协变量包括人口统计学指标、临床表现特征、合并症、估计的肾小球滤过率(eGFR)、主要诊断和入院时的药物治疗。
研究人员观察到入院时钾水平、死亡与心脏停搏之间存在U形关联。然而,在完全调整的模型中,只有高钾血症(5.0-5.5 [OR为1.83; 95%CI为1.34-2.49]和≥5.5mmol/L [OR为2.27; 95%CI为1.57-3.27])与死亡相关,而只有低钾血症(3.0-3.5 [OR为1.63; 95%CI为1.21-2.19]和<3.0mmol/L [OR为2.72; 95%CI为1.56-4.74])与心脏骤停有关。血钾<3.0mmol/L(OR为1.93; 95%CI为1.00-3.76)与新发房颤相关。多变量调整后,血钾与二度或三度房室传导阻滞之间没有关联。主要诊断(ACS亚型或非ACS诊断)或eGFR未改变结果。
由此可见,入院时高钾血症与疑似ACS患者的院内死亡有关,而低钾血症与心脏骤停和新发房颤有关。
原始出处:
JonasFaxén,et al. Potassium levels and risk of in-hospital arrhythmias and mortality in patients admitted with suspected acute coronary syndrome.International Journal of Cardiology.2018. https://doi.org/10.1016/j.ijcard.2018.09.099
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#冠状动脉综合征#
36
#Cardiol#
38
#血钾水平#
46
#死亡风险#
49
#综合征#
32