JNCI;建议对三阴性乳腺癌进行多基因遗传肿瘤panel检测
2018-08-12 肿瘤咨询编辑部 肿瘤威廉亚洲官网
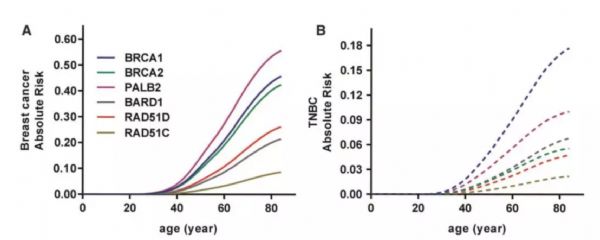
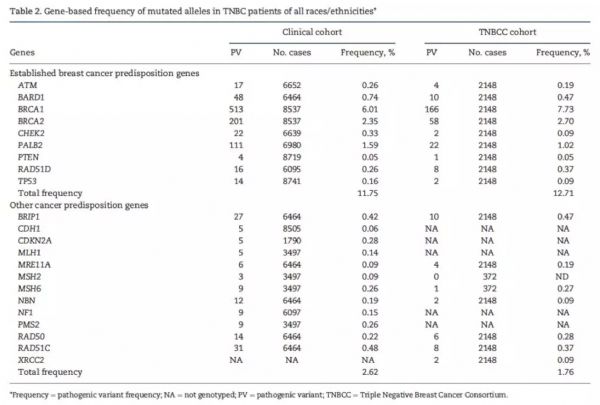
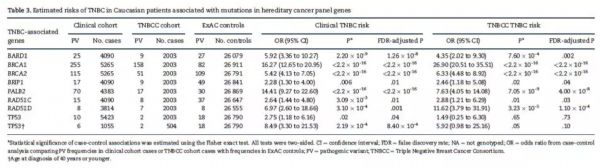
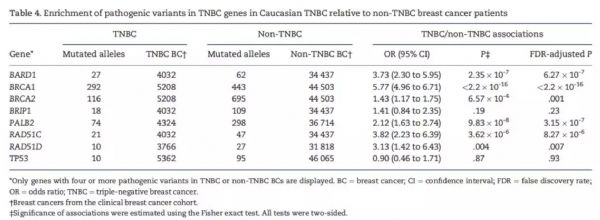
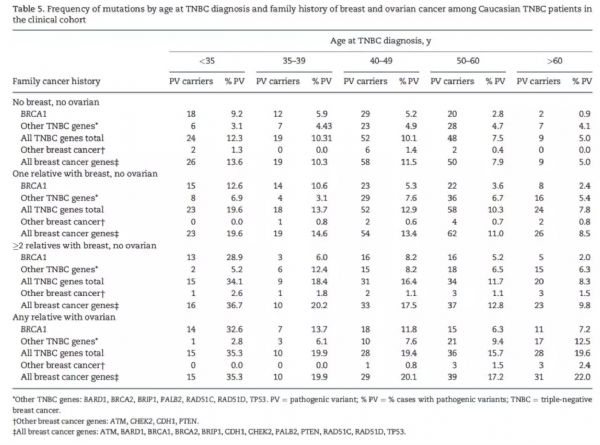
采用遗传肿瘤基因panel检测胚系突变可以发现乳腺癌的高风险人群。然而,与三阴性乳腺癌(TNBC)发表风险相关的基因目前尚未明确,除BRCA1突变外,尚未确立其他的易感基因。近日,发布在JNCI的一项研究旨在确定与TNBC高风险相关的基因检测panel。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#多基因#
69
#NCI#
57
#panel#
73
#阴性乳腺癌#
63
学习学习谢谢
114
#三阴性#
63
学习了,谢谢分享
95