JAMA NEURO:塞莫瑞单抗对轻度阿尔茨海默病及前驱疾病患者的安全性和疗效研究
2022-06-30 MedSci原创 MedSci原创
由聚集的tau蛋白组成的神经纤维缠结是阿尔茨海默病(AD)的神经病理学标志之一,与临床疾病的严重程度相关。
由聚集的tau蛋白组成的神经纤维缠结是阿尔茨海默病(AD)的神经病理学标志之一,与临床疾病的严重程度相关。靶向tau的单克隆抗体可能有潜力通过减缓或停止病理性tau的扩散和/或积累来改善AD的进展。
为了评估单克隆抗tau抗体塞莫瑞单抗对前驱至轻度AD的安全性和有效性,近期,来自美国多家大学的学者开展了相关研究,结果发表在JAMA子刊上。

这项2期随机、双盲、安慰剂对照、平行组临床试验于2017年10月18日至2020年7月16日在北美、欧洲和澳大利亚的97个地点进行。纳入了50至80岁(包括)的前驱至轻度AD患者,MMSE得分在20-30分,并确认了β-淀粉样蛋白病理学。
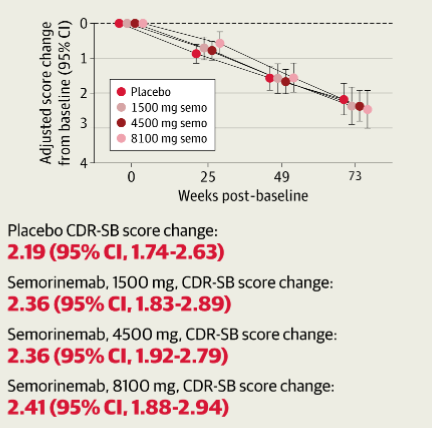
在73周的盲法研究期间,参与者在前3次输液中每2周接受一次安慰剂或塞莫瑞单抗(1500毫克、4500毫克或8100毫克)的静脉输液,此后每4周输液一次。主要结果是,从基线到第73周,临床痴呆评分总分的变化。
结果显示,在修改后的意向性治疗队列中(n = 422;平均[SD]年龄,69.6[7.0]岁;235名女性[55.7%]),安慰剂和塞莫瑞单抗(1500 mg: n = 86; Δ = 2.36 [95% CI, 1.83-2.89]; 4500 mg: n = 126; Δ = 2.36 [95% CI, 1.92-2.79]; 8100 mg: n = 84; Δ = 2.41 [95% CI, 1.88-2.94])的临床痴呆症评分之和得分改变情况类似(n = 126;Δ = 2.19 [95% CI, 1.74-2.63])。
在有安全价值的队列(n = 441)中,安慰剂(130 [93.1%])和塞莫瑞单抗(1500 mg:89 [88.8%];4500 mg:132 [94.7%];8100 mg:90 [92.2%])组出现不良事件的参与者比例相似。
综上,在这项随机临床试验中,与安慰剂相比,在整个73周的研究期间,塞莫瑞单抗并没有减缓临床AD的进展,但确实表现出可接受的和良好耐受的安全性。
参考文献:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言


















#疾病患者#
53
#阿尔茨海#
45
#阿尔茨#
53
#阿尔茨海默#
51
JAMA上文章都是顶级的,谢谢williamhill asia 及时上新
44