NEJM:ICU气管造口术治疗后拔管标准研究
2020-09-10 MedSci原创 MedSci原创
研究认为,对于ICU需接受气管造口术治疗的患者,持续高流量氧疗并以吸氧频率作为是否拔管的指标,相对于间歇性高流量氧疗并以管口封闭作为拔管指标,可缩短拔管时间,降低肺炎和支气管炎风险
对于接受气管造口术治疗的患者,当具备拔管条件后,需进行24小时的管口封闭以评估患者的自主呼吸功能。近日研究人员评估了一种以患者吸氧频率作为拔管指标的临床可行性。
研究在五个重症监护病房(ICU)开展,有意识的重症病人参与,患者接受气管造口术,经治疗后满足脱离机械通气条件。随后患者随机分为24小时管口封闭联合间歇高流量氧疗(对照组)或接受持续高流量氧治疗,以吸氧频率作为是否具备拔管的指标(干预组)。研究的主要结果是拔管时间,次要结果包括拔管失败、呼吸道感染、脓毒症、多器官衰竭、ICU和住院时间以及ICU和院内死亡。
330名患者参与研究,平均年龄为58.3岁,男性患者占68.2%,161名患者分配到对照组,169名患者分配到干预组。干预组的拔管时间短于对照组(中位数,6天 vs 13天;绝对差异为7天)。
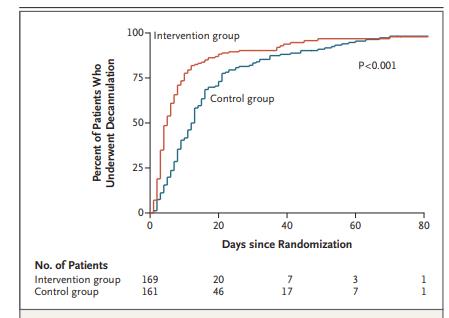
组间拔管时间差异
干预组与对照组相比,肺炎和气管支气管炎的发生率较低,住院时间较短。组间其他次要结果发生率相似。
研究认为,对于ICU需接受气管造口术治疗的患者,持续高流量氧疗并以吸氧频率作为是否拔管的指标,相对于间歇性高流量氧疗并以管口封闭作为拔管指标,可缩短拔管时间,降低肺炎和支气管炎风险。
原始出处:
Gonzalo Hernández Martínez et al. High-Flow Oxygen with Capping or Suctioning for Tracheostomy Decannulation. N Engl J Med, September 10, 2020.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














这个研究好!属于#精准医学#范畴
218
#拔管#
119
#造口术#
115
学习
0
好
148
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
116