虽然晚期肺癌治疗的进展与生存率的适度提高有关,但早期发现肺癌仍然是降低肺癌死亡率的最有希望的战略。在随机对照试验中,使用低剂量计算机断层扫描CT的肺癌筛查已被证明与胸部X光检查或不筛查相比,能在早期发现肺癌。
为了确定2013年引入的低剂量胸部CT筛查对肺癌分期转移、生存率以及美国诊断的肺癌分期的差异的影响,来自哈佛胸心外科的学者开展了一项准实验性研究,结果发表在BMJ杂志上。

该试验使用Joinpoint模型、多变量序数逻辑回归和多变量Cox比例危害模型,使用来自美国国家癌症数据库和监测流行病学最终结果项目数据库的数据。参与者为2010-2018年期间被诊断为非小细胞肺癌(NSCLC)的45-80岁的患者。
在55-80岁的患者中,诊断为I期的NSCLC的比例从2010年到2013年没有明显增加(从27.8%到29.4%),然后从2014年到2018年每年增加3.9%(95%CI:3.0%-4.8%)(从30.2%到35.5%)。在多变量调整分析中,在2014年至2018年的时间段内,患者在诊断时肺癌阶段低一个阶段,每年增加的几率比2010年至2013年每年增加的几率高6.2%(OR=1.062,95%CI:1.048-1.077)。
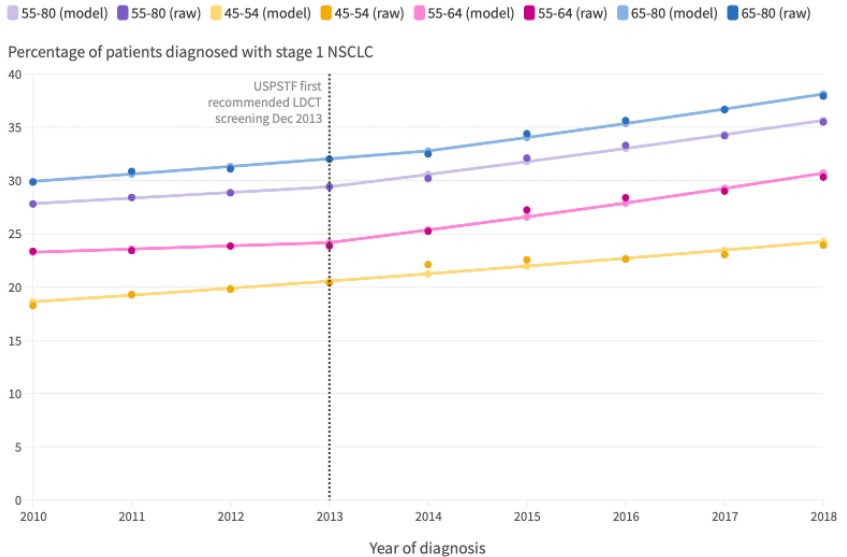
2010年至2018年,不同年龄段患者在诊断时为I期NSCLC的百分比趋势
同样,55-80岁患者的全因生存期中位数从2010年到2013年没有明显增加(从15.8个月到18.1个月),然后从2014年到2018年每年增加11.9%(8.9%-15.0%)(从19.7到28.2个月)。在多变量调整分析中,与2014年之前相比,2014年之后的死亡危险明显下降得更快。从2014年到2018年,美国早期疾病检测的增加减少了10100例死亡。
由此可见,向I期NSCLC的转变与生存率的提高指示应引入肺癌筛查。非白人患者和那些生活在更贫困地区的患者的I期疾病识别率较低,强调了在美国需要努力增加筛查的机会。
参考文献:
Association of computed tomography screening with lung cancer stage shift and survival in the United States: quasi-experimental study. BMJ 2022;376:e069008.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#CT筛查#
74
#BMJ#
69
#胸部CT#
94
#哈佛#
66