JAMA:MRI引导下心房纤维化消融对肺静脉隔离术后心律失常复发风险的影响
2022-06-23 zhangfan MedSci原创
对于持续性房颤患者,与单纯肺静脉隔离相比,MRI引导下纤维化消融联合肺静脉隔离不能降低患者术后房性心律失常复发风险。

持续性房颤(AF)消融仍是临床上的一大挑战,心房性心律失常患者往往复发风险高,需接受多次手术。虽然新技术不断出现,但与传统的肺静脉隔离(PVI)相比,其优势不显著。左心房纤维化是心房肌病的标志特征,在房颤的病理生理过程中起着重要的作用。磁共振成像(MRI)发现,基线左心房纤维化程度与消融后的心房性心律失常复发风险和不良预后独立相关。近日研究人员考察了MRI靶向心房纤维化组织消融对改善持续性房颤患者心律失常复发风险的有效性。
本次研究在10个国家的44个医学中心开展,843名有症状或无症状的持续性房颤患者接受房颤消融治疗,患者随机分为肺静脉隔离(PVI)联合MRI引导的心房纤维化消融(n=421例)或单纯PVI(n=422例)。研究的主要终点为术后90天首次房性心律失常复发,安全性终点事件包括中风、PV狭窄、出血、心力衰竭或死亡。
患者平均年龄62.7岁,178名女性(21.1%),815人(96.9%)完成了术后90天评估。研究发现,组间房性心律失常复发风险无显著差异(纤维化引导消融+PVI组175例vs单纯PVI组188例,43.0% vs 46.1%,HR=0.95)。纤维引导消融+PVI组患者的安全性终点事件发生率更高(9 vs 0例,2.2% vs 0)。纤维化引导消融+PVI组有6名患者(1.5%)发生缺血性卒中,而单纯PVI组无缺血性卒中病例。纤维化引导消融+PVI组有2名患者死亡,其中之一可能与手术有关。
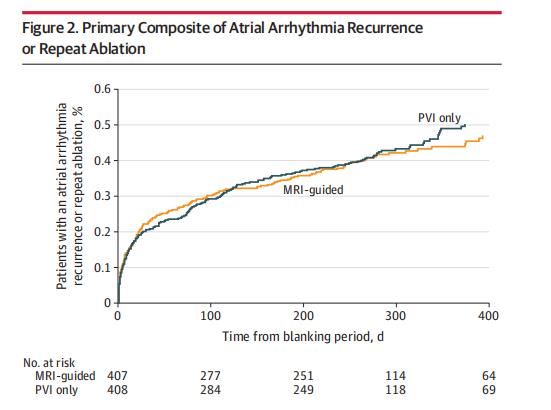
研究认为,对于持续性房颤患者,与单纯肺静脉隔离相比,MRI引导下纤维化消融联合肺静脉隔离不能降低患者术后房性心律失常复发风险。
原始出处:
Nassir F. Marrouche et al. Effect of MRI-Guided Fibrosis Ablation vs Conventional Catheter Ablation on Atrial Arrhythmia Recurrence in Patients With Persistent Atrial Fibrillation The DECAAF II Randomized Clinical Trial. JAMA,21 June 2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#复发风险#
83
#静脉#
72
#肺静脉隔离#
48
#消融#
87
#心房#
57
认真学习~~
61
JAMA上文章都是顶级的,谢谢williamhill asia 及时上新
57