能帮外科医生区分健康或癌变组织的「激光笔」
2015-07-03 shixinxin 煎蛋网
外科医生们用“果冻里取蜘蛛”来形容复杂的脑部肿瘤移除手术。若肿瘤的取出范围太小,癌变细胞的“余党”还会继续作恶——范围太大就会存在误切健康组织,致病人变残疾的风险。 如今英国一家医院正在试用一种像倒车雷达的激光笔,它会在手术刀接近癌变组织边缘的时候发出“哔哔”声,让外科医生清楚误差限度。 英国伦敦帝国学院医疗卫生NHS信托机构的神经外科医生们率先在这一领域使用这种名为Core、像钢笔一样的装置
外科医生们用“果冻里取蜘蛛”来形容复杂的脑部肿瘤移除手术。若肿瘤的取出范围太小,癌变细胞的“余党”还会继续作恶——范围太大就会存在误切健康组织,致病人变残疾的风险。
如今英国一家医院正在试用一种像倒车雷达的激光笔,它会在手术刀接近癌变组织边缘的时候发出“哔哔”声,让外科医生清楚误差限度。 英国伦敦帝国学院医疗卫生NHS信托机构的神经外科医生们率先在这一领域使用这种名为Core、像钢笔一样的装置。该装置会发出近红外线光使肿瘤发亮、扫描鉴别出健康组织和癌变组织的微小差别。 判断可以在一秒钟内完成。当医生的手术刀靠近健康组织,它会马上发出警告声。在英国,每年约有16,000人被确诊患有脑瘤,与其他癌症相比,死于该疾病的患者多为儿童和40岁以下的成年人。该病类型可以被细分为120多种。外科医生们希望借助Core、这一在加拿大皮肤癌手术中已被证明成功有效的装置,能够帮助他们尽可能多地移除癌变组织,同时缩短手术时间。
上周,帝国医院一个脑部手术中这种探针装置被初次使用,假如效果理想的话,在接下来的一年时间里,该装置会应用在30多位患者的手术中。
推进这个项目把Core介绍到英国的高级神经外科实习生Babar Vaqas说:“这是前所未有的时刻。脑部手术非常复杂,一微米的失误都可能引发重大伤害,造成瘫痪或语言功能问题。拥有能让手术更安全更精确的手段才是真正的胜利。”脑部手术面临的困境是,甚至在显微镜下,大脑的癌变组织和正常组织都很难进行区别。外科医生必须依赖对几份微小的组织切片的化验结果来确认他们移除的是否为癌变组织。组织取样化验、等待结果反馈这一过程需耗时90分钟,而此时患者仍然躺在手术室内。
判断可以在一秒钟内完成。当医生的手术刀靠近健康组织,它会马上发出警告声。在英国,每年约有16,000人被确诊患有脑瘤,与其他癌症相比,死于该疾病的患者多为儿童和40岁以下的成年人。该病类型可以被细分为120多种。外科医生们希望借助Core、这一在加拿大皮肤癌手术中已被证明成功有效的装置,能够帮助他们尽可能多地移除癌变组织,同时缩短手术时间。
上周,帝国医院一个脑部手术中这种探针装置被初次使用,假如效果理想的话,在接下来的一年时间里,该装置会应用在30多位患者的手术中。
推进这个项目把Core介绍到英国的高级神经外科实习生Babar Vaqas说:“这是前所未有的时刻。脑部手术非常复杂,一微米的失误都可能引发重大伤害,造成瘫痪或语言功能问题。拥有能让手术更安全更精确的手段才是真正的胜利。”脑部手术面临的困境是,甚至在显微镜下,大脑的癌变组织和正常组织都很难进行区别。外科医生必须依赖对几份微小的组织切片的化验结果来确认他们移除的是否为癌变组织。组织取样化验、等待结果反馈这一过程需耗时90分钟,而此时患者仍然躺在手术室内。

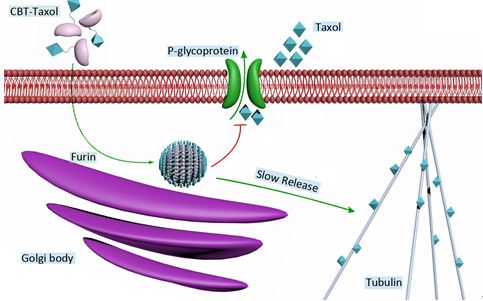
外科医生们认为这种像钢笔一样的探针可以为一般长达3小时的手术时间节约30分钟(模特摆拍) 有了这个装置以后,不用再进行实物取样。医生手拿Core靠近手术区域,探针顶部会发出光束,扫描探寻脑部组织化学成分的变化。光照下,因肿瘤的分子振动不同于健康的组织,所以两者反射的光就会截然不同。探针捕捉到这一差别,把信号传给计算机,随即能够读取出该组织是否为癌变组织。Vaqas先生认为这一装置至少为平均时长为3小时的手术时间缩短了半小时。他说:“不到一秒钟的时间,这个装置就能够区别出健康组织和癌变组织。这还意味着williamhill asia 可以尽量避免不必要的活体组织检查,使手术效率更高。” Core装置制造商, 为加拿大的Verisante技术公司。他们希望帝国医院的手术能够复制多温华一医院的成功。他们用它检测出1,000名皮肤癌患者。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#激光#
51
#外科医生#
53
#癌变#
59
看看
121
好先进
103